Animal lead poisoning
Animal lead poisoning is a significant environmental and health issue affecting both wildlife and domestic animals. Lead, a toxic heavy metal, can be ingested or inhaled by animals, leading to a range of adverse health effects and often resulting in death. This article explores the causes, symptoms, diagnosis, treatment, and prevention of lead poisoning in animals.
Causes[edit | edit source]
Lead poisoning in animals can occur through several pathways. Common sources of lead exposure include:
- Ingestion of Paint Chips: Older buildings may contain lead-based paints. As these paints age and flake off, animals can ingest the chips.
- Contaminated Water: Industrial runoff and old lead pipes can contaminate water sources.
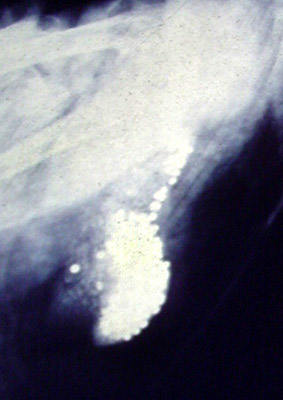
- Lead Shot and Fishing Sinkers: Birds, especially waterfowl, often ingest spent lead shot or fishing sinkers mistaking them for food or grit.
- Mining and Industrial Areas: Animals living near mining sites or industrial areas may be exposed to higher levels of lead in the environment.
- Lead-contaminated Soil: Animals grazing in areas with lead-contaminated soil can ingest lead through the plants they eat.
Symptoms[edit | edit source]
The symptoms of lead poisoning in animals vary depending on the level and duration of exposure. Common symptoms include:
- Gastrointestinal issues such as vomiting and diarrhea
- Neurological problems, including seizures, lack of coordination, and aggressive behavior
- Anemia
- Weight loss and loss of appetite
- Muscle weakness
- Fatigue
In severe cases, lead poisoning can lead to coma and death.
Diagnosis[edit | edit source]
Diagnosis of lead poisoning in animals involves a combination of clinical signs, history of potential exposure, and laboratory tests. Blood tests can measure the lead levels in an animal's system, confirming exposure and aiding in the diagnosis.
Treatment[edit | edit source]
Treatment for lead poisoning in animals focuses on removing the source of lead exposure, supportive care, and specific therapies to reduce lead levels in the body. Treatments may include:
- Chelation Therapy: Medications that bind to lead, allowing it to be excreted from the body.
- Supportive Care: Fluid therapy, nutritional support, and treatment of symptoms such as seizures.
- Environmental Management: Identifying and eliminating the source of lead exposure is crucial to prevent further poisoning.
Prevention[edit | edit source]
Preventing lead poisoning in animals involves reducing their exposure to lead. Measures include:
- Using lead-free paints and removing old lead-based paints from buildings and structures.
- Proper disposal of lead shot and fishing sinkers.
- Ensuring clean, uncontaminated water sources.
- Monitoring and managing industrial emissions and waste.
Conclusion[edit | edit source]
Animal lead poisoning is a preventable condition that poses a significant threat to the health and well-being of both domestic and wild animals. Awareness and proactive management of lead sources in the environment are critical to protecting animal populations from the harmful effects of lead exposure.
Transform your life with W8MD's budget GLP1 injections from $125
W8MD offers a medical weight loss program NYC and a clinic to lose weight in Philadelphia. Our W8MD's physician supervised medical weight loss centers in NYC provides expert medical guidance, and offers telemedicine options for convenience.
Why choose W8MD?
- Comprehensive care with FDA-approved weight loss medications including:
- loss injections in NYC both generic and brand names:
- weight loss medications including Phentermine, Qsymia, Diethylpropion etc.
- Accept most insurances for visits or discounted self pay cost.
- Generic weight loss injections starting from just $125.00 for the starting dose
- In person weight loss NYC and telemedicine medical weight loss options in New York city available
- Budget GLP1 weight loss injections in NYC starting from $125.00 biweekly with insurance!
Book Your Appointment
Start your NYC weight loss journey today at our NYC medical weight loss, and Philadelphia medical weight loss Call (718)946-5500 for NY and 215 676 2334 for PA
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD