Nasopharyngeal carcinoma
(Redirected from Nasopharynx cancer)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Nasopharyngeal carcinoma | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Lump in the neck, hearing loss, nosebleeds, headache, facial pain |
| Complications | Metastasis, cranial nerve palsy |
| Onset | Most common in adults |
| Duration | Chronic |
| Types | N/A |
| Causes | Epstein–Barr virus, genetic factors, environmental factors |
| Risks | Family history, diet, tobacco smoking, alcohol consumption |
| Diagnosis | Nasopharyngoscopy, biopsy, imaging studies |
| Differential diagnosis | Lymphoma, adenocarcinoma, squamous cell carcinoma |
| Prevention | N/A |
| Treatment | Radiation therapy, chemotherapy, surgery |
| Medication | N/A |
| Prognosis | Variable, depends on stage and treatment |
| Frequency | Rare in most parts of the world, more common in East Asia |
| Deaths | N/A |
A type of cancer originating in the nasopharynx

Nasopharyngeal carcinoma (NPC) is a type of cancer that originates in the nasopharynx, which is located behind the nose and above the back of the throat. It is a rare form of cancer in most parts of the world but is more common in certain regions, such as Southeast Asia, North Africa, and the Arctic.
Epidemiology[edit | edit source]
Nasopharyngeal carcinoma is particularly prevalent in southern China, especially in the Guangdong province, as well as in Hong Kong, Taiwan, and other parts of Southeast Asia. It is also more common among the Inuit populations of Alaska and Canada, and among certain ethnic groups in North Africa and the Middle East. The incidence of NPC is higher in males than in females.
Risk Factors[edit | edit source]
Several risk factors have been associated with nasopharyngeal carcinoma:
- Epstein-Barr virus (EBV) infection: There is a strong association between EBV and NPC. The virus is found in the cancer cells of most patients with NPC.
- Genetic predisposition: Family history of NPC increases the risk, suggesting a genetic component.
- Dietary factors: Consumption of salt-cured fish and meats, which contain high levels of nitrosamines, is linked to a higher risk of NPC.
- Environmental factors: Exposure to certain chemicals and dusts, such as formaldehyde and wood dust, may increase the risk.
Symptoms[edit | edit source]
The symptoms of nasopharyngeal carcinoma can vary but often include:
- A lump in the neck due to swollen lymph nodes
- Nasal congestion or blockage
- Nosebleeds
- Hearing loss or ringing in the ears
- Headaches
- Facial pain or numbness
Diagnosis[edit | edit source]
Diagnosis of nasopharyngeal carcinoma typically involves a combination of:
- Physical examination: Checking for lumps in the neck and other symptoms.
- Endoscopy: Using a thin, flexible tube with a camera to view the nasopharynx.
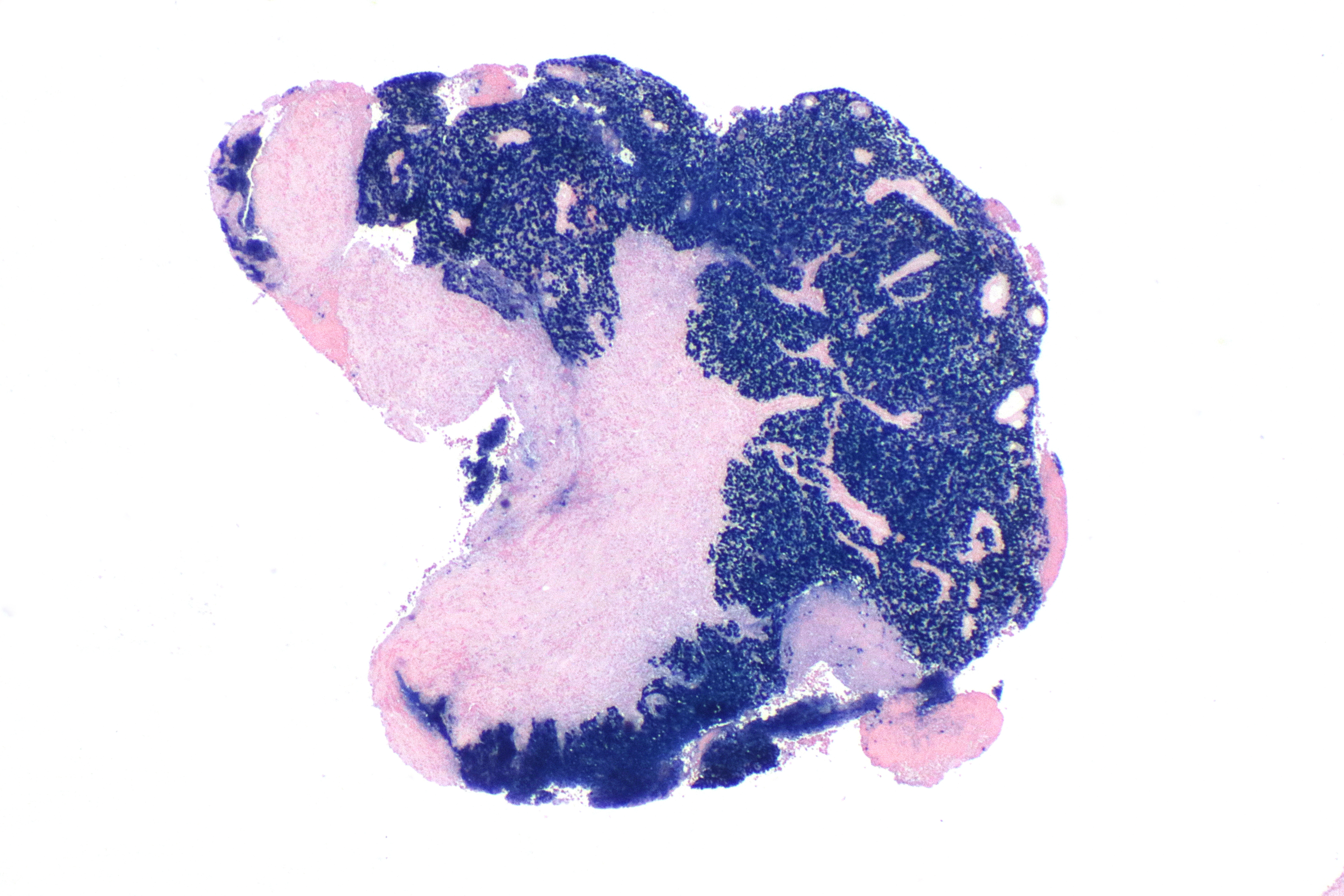
- Biopsy: Taking a tissue sample from the nasopharynx for examination under a microscope.
- Imaging tests: Such as CT scan, MRI, and PET-CT scan to determine the extent of the cancer.
Staging[edit | edit source]
Nasopharyngeal carcinoma is staged based on the size of the tumor, the involvement of lymph nodes, and the presence of metastasis. The stages range from I (localized) to IV (advanced).
Treatment[edit | edit source]
The treatment of nasopharyngeal carcinoma often involves a combination of therapies:
- Radiation therapy: The primary treatment for NPC, often combined with chemotherapy.
- Chemotherapy: Used in conjunction with radiation therapy, especially for advanced stages.
- Surgery: Rarely used as the primary treatment but may be considered for recurrent cases.
Prognosis[edit | edit source]
The prognosis for nasopharyngeal carcinoma depends on the stage at diagnosis and the response to treatment. Early-stage NPC has a better prognosis, while advanced stages may have a poorer outcome.
See also[edit | edit source]
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Kondreddy Naveen, Prab R. Tumpati, MD



