Development of the Fetal Membranes and Placenta
Anatomy > Gray's Anatomy of the Human Body > I. Embryology > 11. Development of the Fetal Membranes and Placenta Henry Gray (1821–1865). Anatomy of the Human Body. 1918.
Development of the Fetal Membranes and Placenta
The Allantois—The allantois arises as a tubular diverticulum of the posterior part of the yolk-sac; when the hind-gut is developed the allantois is carried backward with it and then opens into the cloaca or terminal part of the hind-gut: it grows out into the body-stalk, a mass of mesoderm which lies below and around the tail end of the embryo. The diverticulum is lined by entoderm and covered by mesoderm, and in the latter are carried the allantoic or umbilical vessels.
In reptiles, birds, and many mammals the allantois becomes expanded into a vesicle which projects into the extra-embryonic celom. If its further development be traced in the bird, it is seen to project to the right side of the embryo, and, gradually expanding, it spreads over its dorsal surface as a flattened sac between the amnion and the serosa, and extending in all directions, ultimately surrounds the yolk. Its outer wall becomes applied to and fuses with the serosa, which lies immediately inside the shell membrane.
Blood is carried to the allantoic sac by the two allantoic or umbilical arteries, which are continuous with the primitive aorta, and after circulating through the allantoic capillaries, is returned to the primitive heart by the two umbilical veins. In this way the allantoic circulation, which is of the utmost importance in connection with the respiration and nutrition of the chick, is established. Oxygen is taken from, and carbonic acid is given up to the atmosphere through the egg-shell, while nutritive materials are at the same time absorbed by the blood from the yolk
In man and other primates the nature of the allantois is entirely different from that just described. Here it exists merely as a narrow, tubular diverticulum of the hind-gut, and never assumes the form of a vesicle outside the embryo.
With the formation of the amnion the embryo is, in most animals, entirely separated from the chorion, and is only again united to it when the allantoic mesoderm spreads over and becomes applied to its inner surface.
The human embryo, on the other hand, as was pointed out by His, is never wholly separated from the chorion, its tail end being from the first connected with the chorion by means of a thick band of mesoderm, named the body-stalk (Bauchstiel); into this stalk the tube of the allantois extends .
The Amnion—The amnion is a membranous sac which surrounds and protects the embryo. It is developed in reptiles, birds, and mammals, which are hence called “Amniota;” but not in amphibia and fishes, which are consequently termed “Anamnia.”
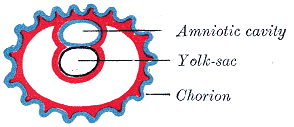
In the human embryo the earliest stages of the formation of the amnion have not been observed; in the youngest embryo which has been studied the amnion was already present as a closed sac (Figs. 24 and 32), and, as indicated on page 46, appears in the inner cell-mass as a cavity.
This cavity is roofed in by a single stratum of flattened, ectodermal cells, the amniotic ectoderm and its floor consists of the prismatic ectoderm of the embryonic disk—the continuity between the roof and floor being established at the margin of the embryonic disk. Outside the amniotic ectoderm is a thin layer of mesoderm, which is continuous with that of the somatopleure and is connected by the body-stalk with the mesodermal lining of the chorion.
When first formed the amnion is in contact with the body of the embryo, but about the fourth or fifth week fluid (liquor amnii) begins to accumulate within it. This fluid increases in quantity and causes the amnion to expand and ultimately to adhere to the inner surface of the chorion, so that the extra-embryonic part of the celom is obliterated.
The liquor amnii increases in quantity up to the sixth or seventh month of pregnancy, after which it diminishes somewhat; at the end of pregnancy it amounts to about 1 liter. It allows of the free movements of the fetus during the later stages of pregnancy, and also protects it by diminishing the risk of injury from without. It contains less than 2 per cent. of solids, consisting of urea and other extractives, inorganic salts, a small amount of protein, and frequently a trace of sugar.
That some of the liquor amnii is swallowed by the fetus is proved by the fact that epidermal debris and hairs have been found among the contents of the fetal alimentary canal. In reptiles, birds, and many mammals the amnion is developed in the following manner: At the point of constriction where the primitive digestive tube of the embryo joins the yolk-sac a reflection or folding upward of the somatopleure takes place.
This, the amniotic fold (Fig. 29), first makes its appearance at the cephalic extremity, and subsequently at the caudal end and sides of the embryo, and gradually rising more and more, its different parts meet and fuse over the dorsal aspect of the embryo, and enclose a cavity, the amniotic cavity After the fusion of the edges of the amniotic fold, the two layers of the fold become completely separated, the inner forming the amnion the outer the false amnion or serosa The space between the amnion and the serosa constitutes the extra-embryonic celom, and for a time communicates with the embryonic celom.
The Umbilical Cord and Body-stalk—The umbilical cord (Fig. 28) attaches the fetus to the placenta; its length at full time, as a rule, is about equal to the length of the fetus, i.e about 50 cm, but it may be greatly diminished or increased.
The rudiment of the umbilical cord is represented by the tissue which connects the rapidly growing embryo with the extra-embryonic area of the ovum. Included in this tissue are the body-stalk and the vitelline duct—the former containing the allantoic diverticulum and the umbilical vessels, the latter forming the communication between the digestive tube and the yolk-sac.
The body-stalk is the posterior segment of the embryonic area, and is attached to the chorion. It consists of a plate of mesoderm covered by thickened ectoderm on which a trace of the neural groove can be seen, indicating its continuity with the embryo. Running through its mesoderm are the two umbilical arteries and the two umbilical veins, together with the canal of the allantois—the last being lined by entoderm (Fig. 31). Its dorsal surface is covered by the amnion, while its ventral surface is bounded by the extra-embryonic celom, and is in contact with the vitelline duct and yolk-sac.
With the rapid elongation of the embryo and the formation of the tail fold, the body stalk comes to lie on the ventral surface of the embryo (Figs. 27 and 28), where its mesoderm blends with that of the yolk-sac and the vitelline duct. The lateral leaves of somatopleure then grow round on each side, and, meeting on the ventral aspect of the allantois, enclose the vitelline duct and vessels, together with a part of the extra-embryonic celom; the latter is ultimately obliterated.
The cord is covered by a layer of ectoderm which is continuous with that of the amnion, and its various constitutents are enveloped by embryonic gelatinous tissue, jelly of Wharton The vitelline vessels and duct, together with the right umbilical vein, undergo atrophy and disappear; and thus the cord, at birth, contains a pair of umbilical arteries and one (the left) umbilical vein.
Implantation or Imbedding of the Ovum—As described , fertilization of the ovum occurs in the lateral or ampullary end of the uterine tube and is immediately followed by segmentation. On reaching the cavity of the uterus the segmented ovum adheres like a parasite to the uterine mucous membrane, destroys the epithelium over the area of contact, and excavates for itself a cavity in the mucous membrane in which it becomes imbedded.
In the ovum described by Bryce and Teacher 7 the point of entrance was visible as a small gap closed by a mass of fibrin and leucocytes; in the ovum described by Peters, 8 the opening was covered by a mushroom-shaped mass of fibrin and blood-clot (Fig. 32), the narrow stalk of which plugged the aperture in the mucous membrane. Soon, however, all trace of the opening is lost and the ovum is then completely surrounded by the uterine mucous membrane.
The structure actively concerned in the process of excavation is the trophoblast of the ovum, which possesses the power of dissolving and absorbing the uterine tissues. The trophoblast proliferates rapidly and forms a network of branching processes which cover the entire ovum and invade and destroy the maternal tissues and open into the maternal bloodvessels, with the result that the spaces in the trophoblastic network are filled with maternal blood; these spaces communicate freely with one another and become greatly distended and form the intervillous space

The Decidua—Before the fertilized ovum reaches the uterus, the mucous membrane of the body of the uterus undergoes important changes and is then known as the decidua The thickness and vascularity of the mucous membrane are greatly increased; its glands are elongated and open on its free surface by funnel-shaped orifices, while their deeper portions are tortuous and dilated into irregular spaces.
The interglandular tissue is also increased in quantity, and is crowded with large round, oval, or polygonal cells, termed decidual cells These changes are well advanced by the second month of pregnancy, when the mucous membrane consists of the following strata (Fig. 33): (1) stratum compactum next the free surface; in this the uterine glands are only slightly expanded, and are lined by columnar cells; (2) stratum spongiosum in which the gland tubes are greatly dilated and very tortuous, and are ultimately separated from one another by only a small amount of interglandular tissue, while their lining cells are flattened or cubical; (3) a thin unaltered or boundary layer next the uterine muscular fibers, containing the deepest parts of the uterine glands, which are not dilated, and are lined with columnar epithelium; it is from this epithelium that the epithelial lining of the uterus is regenerated after pregnancy.
Distinctive names are applied to different portions of the decidua. The part which covers in the ovum is named the decidua capsularis; the portion which intervenes between the ovum and the uterine wall is named the decidua basalis or decidua placentalis; it is here that the placenta is subsequently developed.
The part of the decidua which lines the remainder of the body of the uterus is known as the decidua vera or decidua parietalis Coincidently with the growth of the embryo, the decidua capsularis is thinned and extended (Fig. 34) and the space between it and the decidua vera is gradually obliterated, so that by the third month of pregnancy the two are in contact.
By the fifth month of pregnancy the decidua capsularis has practically disappeared, while during the succeeding months the decidua vera also undergoes atrophy, owing to the increased pressure.
The glands of the stratum compactum are obliterated, and their epithelium is lost. In the stratum spongiosum the glands are compressed and appear as slit-like fissures, while their epithelium undergoes degeneration. In the unaltered or boundary layer, however, the glandular epithelium retains a columnar or cubical form.
The Chorion—The chorion consists of two layers: an outer formed by the primitive ectoderm or trophoblast, and an inner by the somatic mesoderm; with this latter the amnion is in contact. The trophoblast is made up of an internal layer of cubical or prismatic cells, the cytotrophoblast or layer of Langhans and an external layer of richly nucleated protoplasm devoid of cell boundaries, the syncytiotrophoblast It undergoes rapid proliferation and forms numerous processes, the chorionic villi which invade and destroy the uterine decidua and at the same time absorb from it nutritive materials for the growth of the embryo.
The chorionic villi are at first small and non-vascular, and consist of trophoblast only, but they increase in size and ramify, while the mesoderm, carrying branches of the umbilical vessels, grows into them, and in this way they are vascularized.
Blood is carried to the villi by the branches of the umbilical arteries, and after circulating through the capillaries of the villi, is returned to the embryo by the umbilical veins. Until about the end of the second month of pregnancy the villi cover the entire chorion, and are almost uniform in size (Fig. 25), but after this they develop unequally.
The greater part of the chorion is in contact with the decidua capsularis (Fig. 34), and over this portion the villi, with their contained vessels, undergo atrophy, so that by the fourth month scarcely a trace of them is left, and hence this part of the chorion becomes smooth, and is named the chorion læve; as it takes no share in the formation of the placenta, it is also named the non-placental part of the chorion.
On the other hand, the villi on that part of the chorion which is in contact with the decidua placentalis increase greatly in size and complexity, and hence this part is named the chorion frondosum (Fig. 28).
The Placenta—The placenta connects the fetus to the uterine wall, and is the organ by means of which the nutritive, respiratory, and excretory functions of the fetus are carried on. It is composed of fetal and maternal portions.
Fetal Portion—The fetal portion of the placenta consists of the villi of the chorion frondosum; these branch repeatedly, and increase enormously in size. These greatly ramified villi are suspended in the intervillous space, and are bathed in maternal blood, which is conveyed to the space by the uterine arteries and carried away by the uterine veins.
A branch of an umbilical artery enters each villus and ends in a capillary plexus from which the blood is drained by a tributary of the umbilical vein.
The vessels of the villus are surrounded by a thin layer of mesoderm consisting of gelatinous connective tissue, which is covered by two strata of ectodermal cells derived from the trophoblast: the deeper stratum, next the mesodermic tissue, represents the cytotrophoblast or layer of Langhans; the superficial, in contact with the maternal blood, the syncytiotrophoblast (Figs. 36 and 37).
After the fifth month the two strata of cells are replaced by a single layer of somewhat flattened cells.
Maternal Portion—The maternal portion of the placenta is formed by the decidua placentalis containing the intervillous space. As already explained, this space is produced by the enlargement and intercommunication of the spaces in the trophoblastic network.
The changes involve the disappearance of the greater portion of the stratum compactum, but the deeper part of this layer persists and is condensed to form what is known as the basal plate Between this plate and the uterine muscular fibres are the stratum spongiosum and the boundary layer; through these and the basal plate the uterine arteries and veins pass to and from the intervillous space.
The endothelial lining of the uterine vessels ceases at the point where they terminate in the intervillous space which is lined by the syncytiotrophoblast.
Portions of the stratum compactum persist and are condensed to form a series of septa, which extend from the basal plate through the thickness of the placenta and subdivide it into the lobules or cotyledons seen on the uterine surface of the detached placenta.
The fetal and maternal blood currents traverse the placenta, the former passing through the bloodvessels of the placental villi and the latter through the intervillous space (Fig. 39). The two currents do not intermingle, being separated from each other by the delicate walls of the villi.
Nevertheless, the fetal blood is able to absorb, through the walls of the villi, oxygen and nutritive materials from the maternal blood, and give up to the latter its waste products.
The blood, so purified, is carried back to the fetus by the umbilical vein. It will thus be seen that the placenta not only establishes a mechanical connection between the mother and the fetus, but subserves for the latter the purposes of nutrition, respiration, and excretion. In favor of the view that the placenta possesses certain selective powers may be mentioned the fact that glucose is more plentiful in the maternal than in the fetal blood.
It is interesting to note also that the proportion of iron, and of lime and potash, in the fetus is increased during the last months of pregnancy. Further, there is evidence that the maternal leucocytes may migrate into the fetal blood, since leucocytes are much more numerous in the blood of the umbilical vein than in that of the umbilical arteries.
The placenta is usually attached near the fundus uteri, and more frequently on the posterior than on the anterior wall of the uterus. It may, however, occupy a lower position and, in rare cases, its site is close to the orificium internum uteri, which it may occlude, thus giving rise to the condition known as placenta previa
Separation of the Placenta—After the child is born, the placenta and membranes are expelled from the uterus as the after-birth The separation of the placenta from the uterine wall takes place through the stratum spongiosum, and necessarily causes rupture of the uterine vessels.
The orifices of the torn vessels are, however, closed by the firm contraction of the uterine muscular fibers, and thus postpartum hemorrhage is controlled. The epithelial lining of the uterus is regenerated by the proliferation and extension of the epithelium which lines the persistent portions of the uterine glands in the unaltered layer of the decidua.
The expelled placenta appears as a discoid mass which weighs about 450 gm. and has a diameter of from 15 to 20 cm. Its average thickness is about 3 cm., but this diminishes rapidly toward the circumference of the disk, which is continuous with the membranes. Its uterine surface is divided by a series of fissures into Iobules or cotyledons the fissures containing the remains of the septa which extended between the maternal and fetal portions.
Most of these septa end in irregular or pointed processes; others, especially those near the edge of the placenta, pass through its thickness and are attached to the chorion. In the early months these septa convey branches of the uterine arteries which open into the intervillous space on the surfaces of the septa.
The fetal surface of the placenta is smooth, being closely invested by the amnion. Seen through the latter, the chorion presents a mottled appearance, consisting of gray, purple, or yellowish areas.
The umbilical cord is usually attached near the center of the placenta, but may be inserted anywhere between the center and the margin; in some cases it is inserted into the membranes, the velamentous insertion From the attachment of the cord the larger branches of the umbilical vessels radiate under the amnion, the veins being deeper and larger than the arteries.
The remains of the vitelline duct and yolk-sac may be sometimes observed beneath the amnion, close to the cord, the former as an attenuated thread, the latter as a minute sac. On section, the placenta presents a soft, spongy appearance, caused by the greatly branched villi; surrounding them is a varying amount of maternal blood giving the dark red color to the placenta.
Many of the larger villi extend from the chorionic to the decidual surface, while others are attached to the septa which separate the cotyledons; but the great majority of the villi hang free in the intervillous space.
Contribution to the study of the early development and imbedding of the human ovum, 1908.Die Einbettung des menschlichen Eies, 1899. [back] == Gray's Anatomy ==
- Gray's Anatomy Contents
- Gray's Anatomy Subject Index
- About Classic Gray's Anatomy
- Glossary of anatomy terms
Anatomy atlases (external)[edit source]
[1] - Anatomy Atlases
| This article is a medical stub. You can help WikiMD by expanding it! | |
|---|---|
| Human systems and organs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Anish, Deepika vegiraju, Prab R. Tumpati, MD