Ménière's disease
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Ménière's disease | |
|---|---|
| |
| Synonyms | Idiopathic endolymphatic hydrops |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Vertigo, tinnitus, hearing loss, ear fullness |
| Complications | N/A |
| Onset | Typically between 20 and 50 years of age |
| Duration | Long-term |
| Types | N/A |
| Causes | Unknown |
| Risks | Family history, autoimmune disorders, allergies |
| Diagnosis | Based on symptoms, audiometry, electrocochleography, MRI |
| Differential diagnosis | Vestibular migraine, acoustic neuroma, labyrinthitis |
| Prevention | N/A |
| Treatment | Vestibular rehabilitation, hearing aids, medications |
| Medication | Diuretics, antihistamines, benzodiazepines |
| Prognosis | Variable; can lead to permanent hearing loss |
| Frequency | 0.2% of the population |
| Deaths | N/A |
Other Names: Meniere's disease; Meniere disease
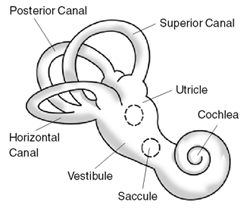
Ménière disease is a disorder of the inner ear that affects balance and hearing. This condition is characterized by sudden episodes of extreme dizziness (vertigo), a roaring sound in the ears (tinnitus), a feeling of pressure or fullness in the ears, and fluctuations in hearing.
Age distribution[edit | edit source]
Ménière disease usually appears in adulthood, most often in a person's 40s or 50s. It is much less common in children and young adults. The symptoms of the disorder typically begin in one ear, although they may later involve both ears.

Epidemiology[edit | edit source]
The prevalence of Ménière disease varies in different geographic regions and ethnic groups. It appears to be more common in people of European descent than in those with other backgrounds. In the United States, there are an estimated 615,000 people with Ménière disease, and more than 45,000 new cases are diagnosed each year.
Cause[edit | edit source]
The cause of Ménière disease is unknown, although it probably results from a combination of environmental and genetic factors. Ménière disease is thought to be related to abnormalities of the inner ear, which contains structures that are needed for normal hearing and balance. Episodes of vertigo, tinnitus, and hearing loss likely result from fluctuating amounts of fluid in the inner ear. These changes disrupt signals sent from the inner ear to the brain that are related to sound and the body's position and movement. Researchers have studied many possible risk factors for Ménière disease, including viral infections, trauma to the inner ear, noise pollution, allergies, abnormal immune system responses, and migraines. Studies have also examined changes in more than a dozen genes that might contribute to the signs and symptoms of this condition. However, none of the factors studied so far appears to play a major role in Ménière disease. Researchers are looking for additional environmental and genetic factors that are associated with this complex disorder.
Inheritance[edit | edit source]
Most cases of Ménière disease are sporadic, which means they occur in people with no history of the disorder in their family. A small percentage of all cases have been reported to run in families. When the disorder is familial, it most often has an autosomal dominant pattern of inheritance. Autosomal dominant inheritance means one copy of an altered gene in each cell is sufficient to increase the risk of the disorder. However, no associated genes have been identified.
Signs and symptoms[edit | edit source]
The symptoms of Ménière's disease typically occur suddenly and may be experienced daily, or as infrequently as once a year. Vertigo, often the most debilitating symptom of Ménière's disease, typically involves a whirling dizziness that forces the affected person to lie down. Vertigo attacks can lead to severe nausea, vomiting, and sweating, and often come with little or no warning. Some people with Ménière's disease have attacks that start with tinnitus (ear noises), a loss of hearing, or a full feeling or pressure in the affected ear. It is important to remember that all of these symptoms are unpredictable. Typically, the attack is characterized by a combination of vertigo, tinnitus, and hearing loss lasting several hours. People experience these discomforts at varying frequencies, durations, and intensities. Some may feel slight vertigo a few times a year. Others may be occasionally disturbed by intense, uncontrollable tinnitus while sleeping. Affected people may also notice hearing loss or feel unsteady for prolonged periods. Other occasional symptoms of Ménière's disease may include headaches, abdominal discomfort, and diarrhea. A person's hearing tends to recover between attacks but over time may become worse. Meniere's disease usually starts in one ear but it may extend to involve both ears over time.
Diagnosis[edit | edit source]
A diagnosis of Ménière's disease is often suspected based on the presence of characteristic signs and symptoms. These may include:
- Two or more episodes of vertigo lasting at least 20 min each
- Tinnitus
- Temporary hearing loss
- A feeling of fullness in the ear
Proper diagnosis of Ménière's disease entails several procedures, including a medical history interview; a physical examination; hearing and balance tests; and medical imaging with magnetic resonance imaging (MRI). Accurate measurement and characterization of hearing loss are of critical importance in the diagnosis of Ménière's disease. Through the use of several types of hearing tests, physicians can characterize hearing loss as being sensory (arising from the inner ear) or neural (arising from the hearing nerve). Recording the auditory brain stem response, which measures electrical activity in the hearing nerve and brain stem, is useful in differentiating between these two types of hearing loss. Electrocochleography, recording the electrical activity of the inner ear in response to sound, helps confirm the diagnosis. To test the vestibular or balance system, physicians irrigate the ears with warm and cool water or air. This procedure, known as caloric testing, results in nystagmus, rapid eye movements that can help a physician analyze a balance disorder. Since tumor growth can produce symptoms similar to Ménière's disease, an MRI is a useful test to determine whether a tumor is causing the patient's vertigo and hearing loss.
Treatment[edit | edit source]
Ménière‚Äôs disease does not have a cure yet, but your doctor might recommend some of the treatments below to help you cope with the condition. Medications. The most disabling symptom of an attack of Ménière‚Äôs disease is dizziness. Prescription drugs such as meclizine, diazepam, glycopyrrolate, and lorazepam can help relieve dizziness and shorten the attack. Salt restriction and diuretics. Limiting dietary salt and taking diuretics (water pills) help some people control dizziness by reducing the amount of fluid the body retains, which may help lower fluid volume and pressure in the inner ear. Other dietary and behavioral changes. Some people claim that caffeine, chocolate, and alcohol make their symptoms worse and either avoid or limit them in their diet. Not smoking also may help lessen the symptoms. Cognitive therapy. Cognitive therapy is a type of talk therapy that helps people focus on how they interpret and react to life experiences. Some people find that cognitive therapy helps them cope better with the unexpected nature of attacks and reduces their anxiety about future attacks. Injections. Injecting the antibiotic gentamicin into the middle ear helps control vertigo but significantly raises the risk of hearing loss because gentamicin can damage the microscopic hair cells in the inner ear that help us hear. Some doctors inject a corticosteroid instead, which often helps reduce dizziness and has no risk of hearing loss. Pressure pulse treatment. The U.S. Food and Drug Administration (FDA) recently approved a device for Ménière‚Äôs disease that fits into the outer ear and delivers intermittent air pressure pulses to the middle ear. The air pressure pulses appear to act on endolymph fluid to prevent dizziness.
Surgery. Surgery may be recommended when all other treatments have failed to relieve dizziness. Some surgical procedures are performed on the endolymphatic sac to decompress it. Another possible surgery is to cut the vestibular nerve, although this occurs less frequently. Alternative medicine. Although scientists have studied the use of some alternative medical therapies in Ménière‚Äôs disease treatment, there is still no evidence to show the effectiveness of such therapies as acupuncture or acupressure, tai chi, or herbal supplements such as gingko biloba, niacin, or ginger root. Be sure to tell your doctor if you are using alternative therapies, since they sometimes can impact the effectiveness or safety of conventional medicines.
Prognosis[edit | edit source]
Scientists estimate that six out of 10 people either get better on their own or can control their vertigo with diet, drugs, or devices. However, a small group of people with Ménière‚Äôs disease will get relief only by undergoing surgery.
Frequently asked questions[edit | edit source]
- What triggers Meniere's disease?
- What is the best treatment for Meniere's disease?
- Does Meniere's disease go away?
- What not to eat when you have Meniere's?
- What does a Meniere's attack feel like?
- Is Meniere's a disability?
- Can you drive with Meniere's?
- Can you live a normal life with Meniere's disease?
- Can weather affect Meniere's disease?
- What are the three stages of Meniere's disease?
- Does everyone with Meniere's go deaf?
- Does Meniere's get worse with age?
- Is it bad to sleep with earplugs every night?
- Does drinking water help Meniere's disease?
- How do you stop Meniere's attacks?
- How do doctors diagnose Meniere's disease?
- Does Meniere's affect eyesight?
| Disorders of hearing and balance | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info[edit source]
Ménière's disease is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Ménière's disease
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD

