Guanidinoacetate methyltransferase deficiency
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Guanidinoacetate methyltransferase deficiency | |
|---|---|
| |
| Synonyms | GAMT deficiency |
| Pronounce | |
| Specialty | Medical genetics |
| Symptoms | Developmental delay, seizures, extrapyramidal symptoms, intellectual disability |
| Complications | N/A |
| Onset | Infancy |
| Duration | Lifelong |
| Types | N/A |
| Causes | Mutations in the GAMT gene |
| Risks | |
| Diagnosis | Genetic testing, magnetic resonance spectroscopy |
| Differential diagnosis | Cerebral creatine deficiency syndromes |
| Prevention | |
| Treatment | Creatine supplementation, dietary modification |
| Medication | |
| Prognosis | Variable |
| Frequency | Rare |
| Deaths | |
A rare metabolic disorder affecting creatine synthesis
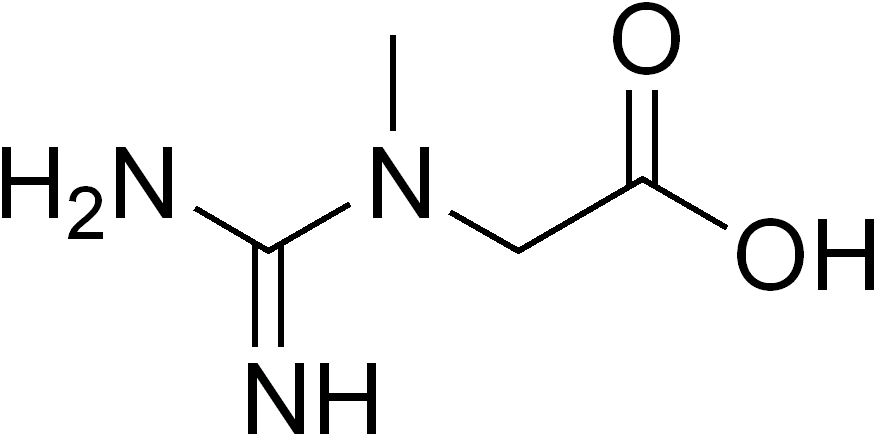
Guanidinoacetate methyltransferase deficiency (GAMT deficiency) is a rare autosomal recessive metabolic disorder that affects the body's ability to synthesize creatine, an essential compound for energy storage and utilization in muscle and brain tissues. This condition is characterized by a deficiency in the enzyme guanidinoacetate methyltransferase, which is crucial for the conversion of guanidinoacetate to creatine.
Pathophysiology[edit | edit source]
Guanidinoacetate methyltransferase deficiency results from mutations in the GAMT gene, which encodes the enzyme responsible for the methylation of guanidinoacetate to form creatine. This enzymatic step is the final stage in the creatine synthesis pathway. The deficiency leads to an accumulation of guanidinoacetate and a depletion of creatine in the body. Elevated levels of guanidinoacetate are neurotoxic and contribute to the neurological symptoms observed in affected individuals.
Clinical Presentation[edit | edit source]
The clinical manifestations of GAMT deficiency typically appear in infancy or early childhood. Common symptoms include:
- Developmental delay
- Intellectual disability
- Seizures
- Hypotonia
- Movement disorders
- Behavioral problems such as autism spectrum disorder-like features
Diagnosis[edit | edit source]
Diagnosis of guanidinoacetate methyltransferase deficiency is based on clinical evaluation, biochemical testing, and genetic analysis. Key diagnostic tests include:
- Measurement of guanidinoacetate and creatine levels in urine and blood
- Magnetic resonance spectroscopy (MRS) to assess brain creatine levels
- Genetic testing to identify mutations in the GAMT gene
Treatment[edit | edit source]
The primary treatment for GAMT deficiency involves dietary supplementation to restore creatine levels and reduce guanidinoacetate accumulation. Treatment strategies include:
- Creatine monohydrate supplementation
- Ornithine supplementation to reduce guanidinoacetate production
- Dietary restriction of arginine and protein to lower guanidinoacetate levels
Early diagnosis and treatment are crucial to improving outcomes and preventing irreversible neurological damage.
Prognosis[edit | edit source]
With early and appropriate treatment, individuals with GAMT deficiency can experience significant improvements in symptoms and quality of life. However, untreated or late-diagnosed cases may result in severe intellectual disability and persistent neurological issues.
See also[edit | edit source]
Transform your life with W8MD's budget GLP1 injections from $125
W8MD offers a medical weight loss program NYC and a clinic to lose weight in Philadelphia. Our W8MD's physician supervised medical weight loss centers in NYC provides expert medical guidance, and offers telemedicine options for convenience.
Why choose W8MD?
- Comprehensive care with FDA-approved weight loss medications including:
- loss injections in NYC both generic and brand names:
- weight loss medications including Phentermine, Qsymia, Diethylpropion etc.
- Accept most insurances for visits or discounted self pay cost.
- Generic weight loss injections starting from just $125.00 for the starting dose
- In person weight loss NYC and telemedicine medical weight loss options in New York city available
- Budget GLP1 weight loss injections in NYC starting from $125.00 biweekly with insurance!
Book Your Appointment
Start your NYC weight loss journey today at our NYC medical weight loss, and Philadelphia medical weight loss Call (718)946-5500 for NY and 215 676 2334 for PA
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD



