Myotonic dystrophy
(Redirected from Proximal myotonic dystrophy)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Myotonic dystrophy | |
|---|---|
| |
| Synonyms | DM, dystrophia myotonica |
| Pronounce | |
| Specialty | Neurology, Genetics |
| Symptoms | Muscle weakness, myotonia, cataracts, cardiac conduction defects, endocrine changes |
| Complications | N/A |
| Onset | Adulthood or childhood |
| Duration | Chronic |
| Types | N/A |
| Causes | Genetic mutation in the DMPK or CNBP gene |
| Risks | Family history |
| Diagnosis | Genetic testing, electromyography |
| Differential diagnosis | Other muscular dystrophies, myopathies |
| Prevention | N/A |
| Treatment | Symptomatic treatment, physical therapy, cardiac monitoring |
| Medication | Mexiletine, phenytoin, quinine |
| Prognosis | N/A |
| Frequency | 1 in 8,000 |
| Deaths | |
Alternate names[edit | edit source]
Dystrophia myotonica; Myotonia atrophica; Myotonia dystrophica
Definition[edit | edit source]
Myotonic dystrophy is a disease that affects the muscles and other body systems. Myotonic dystrophy is part of a group of inherited disorders called muscular dystrophies. It is the most common form of muscular dystrophy that begins in adulthood.
Types[edit | edit source]
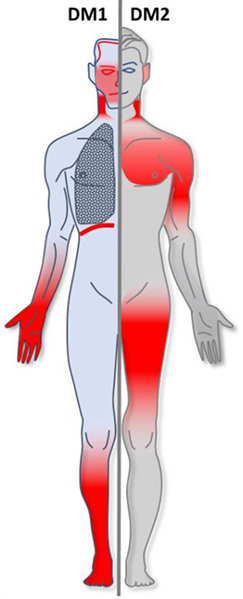
- There are two types of myotonic dystrophy: myotonic dystrophy type 1 and myotonic dystrophy type 2.
- The symptoms in people with myotonic dystrophy type 2 tend to be milder than in those with type 1, but the symptoms may overlap.
- People with myotonic dystrophy type 1 typically experience involvement of the legs, hands, neck, and face, while people with myotonic dystrophy type 2 typically experience involvement of the neck, shoulders, elbows, and hips.
Epidemiology[edit | edit source]
- Myotonic dystrophy affects at least 1 in 8,000 people worldwide.
- The prevalence of the two types of myotonic dystrophy varies among different geographic and ethnic populations.
- In most populations, type 1 appears to be more common than type 2. However, recent studies suggest that type 2 may be as common as type 1 among people in Germany and Finland.
Cause[edit | edit source]
- Myotonic dystrophy type 1 is caused by mutations in the DMPK gene, while type 2 results from mutations in the CNBP gene.
- The protein produced from the DMPK gene likely plays a role in communication within cells.
- It appears to be important for the correct functioning of cells in the heart, brain, and skeletal muscles (which are used for movement).
- The protein produced from the CNBP gene is found primarily in the heart and in skeletal muscles, where it helps regulate the function of other genes.
Gene mutations[edit | edit source]
- Similar changes in the structure of the DMPK and CNBP genes cause myotonic dystrophy type 1 and type 2.
- In each case, a segment of DNA is abnormally repeated many times, forming an unstable region in the gene.
- The gene with the abnormal segment produces an unusually long messenger RNA, which is a molecular blueprint of the gene that guides the production of proteins.
- The unusually long messenger RNA forms clumps inside the cell that interfere with the production of many other proteins.
- These changes prevent muscle cells and cells in other tissues from functioning normally, which leads to the signs and symptoms of myotonic dystrophy.
- If these changes affect the DMPK gene, the result is myotonic dystrophy type 1, if the CNBP gene is affected, the result is myotonic dystrophy type 2.
Inheritance[edit | edit source]
- Both types of myotonic dystrophy are inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person has one parent with the condition.
- As myotonic dystrophy is passed from one generation to the next, the disorder generally begins earlier in life and signs and symptoms become more severe.
- This phenomenon is called anticipation.
- The evidence for anticipation appears only in myotonic dystrophy type 1.
- In this form of the disorder, anticipation is caused by an increase in the length of the unstable region in the DMPK gene. A longer unstable region in the CNBP gene does not appear to influence the age of onset of myotonic dystrophy type 2.
Onset[edit | edit source]
Signs and symptoms of myotonic dystrophy often begin in a person’s 20s or 30s but can begin at any age.
Signs and symptoms[edit | edit source]
- People with this disorder often have prolonged muscle contractions (myotonia) and are not able to relax certain muscles after use.
- For example, a person may have difficulty releasing their grip on a doorknob or handle.
- Also, affected people may have slurred speech or temporary locking of their jaw.
- Other signs and symptoms of myotonic dystrophy include clouding of the lens of the eye (cataracts) and abnormalities of the electrical signals that control the heartbeat (cardiac conduction defects).
- Some affected individuals develop a condition called diabetes mellitus, in which blood sugar levels can become dangerously high.
- The features of myotonic dystrophy often develop during a person's twenties or thirties, although they can occur at any age.
- The severity of the condition varies widely among affected people, even among members of the same family.
- There are two variations of myotonic dystrophy type 1: the mild and congenital types.
- Mild myotonic dystrophy is apparent in mid to late adulthood. Affected individuals typically have mild myotonia and cataracts.
- Congenital myotonic dystrophy is often apparent at birth.
- Characteristic features include weak muscle tone (hypotonia), an inward- and upward-turning foot (clubfoot), breathing problems, delayed development, and intellectual disability. Some of these health problems can be life-threatening.
Diagnosis[edit | edit source]
- Myotonic dystrophy is diagnosed by doing a physical exam.
- A physical exam can identify the typical pattern of muscle wasting and weakness of the jaw and neck muscles and the presence of myotonia. Men may have frontal balding.
- There are several laboratory tests that can be used to clarify the clinical diagnosis of myotonic dystrophy.
- One test, called electromyography (EMG), involves inserting a small needle into the muscle.
- The electrical activity of the muscle is studied and usually shows characteristic patterns of myotonic dystrophy.
- Other laboratory tests may include a muscle biopsy, which can be used to determine if the muscle fibers are weaker than they should be (atrophied), or a blood test to determine if there are elevated levels of certain muscle enzymes.
- The definitive test for myotonic dystrophy is a genetic test.
- For this test, a blood or saliva sample is analyzed to determine if there is a mutation in the DMPK or CNBP (ZNF9) genes.
Treatment[edit | edit source]
- There is currently no cure or specific treatment for myotonic dystrophy.
- Treatment is aimed at managing symptoms of the disease.
- Routine physical activity appears to help maintain muscle strength and endurance and to control musculoskeletal pain.
- Canes, braces, walkers, and scooters can help as muscle weakness progresses.
- There are also medications that can lessen pain associated with myotonic dystrophy.
- Pain management can be achieved through the use of medications prescribed by a doctor.
- Heart problems associated with myotonic dystrophy can be treated through the insertion of a pacemaker, medications, and regular monitoring of cardiac function. Cataracts can be surgically removed. Testosterone replacement therapy may be used to treat infertility in males.
- Current research is focusing on how we might be able to one day use gene-editing technology or other treatments to remove the clumps of RNA that cause the symptoms of myotonic dystrophy. However, this therapy is not yet possible in humans.
Prognosis[edit | edit source]
- The long-term outlook (prognosis) for each person with myotonic dystrophy (including life expectancy) may depend on the type of myotonic dystrophy and the specific medical problems present. Myotonic dystrophy is a progressive disease, meaning that symptoms worsen as a person gets older.
- Although evidence is limited, life expectancy appears to be reduced for people with myotonic dystrophy type 1 (DM1). The most common causes of death in people with DM1 are respiratory and cardiac (heart) symptoms. An increased risk of death may be associated with younger age of onset, more severe muscle weakness, and cardiac conduction defects. People with more mild symptoms of DM1 may have a normal lifespan.
- Definitive information about prognosis in people with myotonic dystrophy type 2 is limited, but the condition generally runs a milder course. People with myotonic dystrophy type 2 may have a normal lifespan.
- While mobility may be impaired at an early age, the ability to walk is often retained until around 60-years-old.
| Muscular dystrophy | ||||||||
|---|---|---|---|---|---|---|---|---|
* Category
|
| Diseases of muscle, neuromuscular junction, and neuromuscular disease | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Non-Mendelian inheritance: anticipation | ||||||
|---|---|---|---|---|---|---|
|
| Deficiencies of intracellular signaling peptides and proteins | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Genetic disorders relating to deficiencies of transcription factor or coregulators | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info[edit source]
Myotonic dystrophy is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Myotonic dystrophy
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD




