The Large Intestine
Anatomy > Gray's Anatomy of the Human Body > XI. Splanchnology > 2h. The Large Intestine
Henry Gray (1821–1865). Anatomy of the Human Body. 1918.
The Large Intestine[edit | edit source]
(Intestinum Crassum)
The large intestine extends from the end of the ileum to the anus. It is about 1.5 meters long, being one-fifth of the whole extent of the intestinal canal. Its caliber is largest at its commencement at the cecum, and gradually diminishes as far as the rectum, where there is a dilatation of considerable size just above the anal canal. It differs from the small intestine in its greater caliber, its more fixed position, its sacculated form, and in possessing certain appendages to its external coat, the appendices epiploicae Further, its longitudinal muscular fibers do not form a continuous layer around the gut, but are arranged in three longitudinal bands or taeniae
The large intestine, in its course, describes an arch which surrounds the convolutions of the small intestine. It commences in the right iliac region, in a dilated part, the cecum It ascends through the right lumbar and hypochondriac regions to the under surface of the liver; it here takes a bend, the right colic flexure to the left and passes transversely across the abdomen on the confines of the epigastric and umbilical regions, to the left hypochondriac region; it then bends again, the left colic flexure and descends through the left lumbar and iliac regions to the pelvis, where it forms a bend called the sigmoid flexure from this it is continued along the posterior wall of the pelvis to the anus.
The large intestine is divided into the cecum, colon, rectum and anal canal
The Cecum[edit | edit source]
The Cecum (intestinum caecum) (Fig. 1073), the commencement of the large intestine, is the large blind pouch situated below the colic valve. Its blind end is directed downward, and its open end upward, communicating directly with the colon, of which this blind pouch appears to be the beginning or head, and hence the old name of caput caecum coli was applied to it. Its size is variously estimated by different authors, but on an average it may be said to be 6.25 cm. in length and 7.5 in breadth. It is situated in the right iliac fossa, above the lateral half of the inguinal ligament: it rests on the Iliacus and Psoas major, and usually lies in contact with the anterior abdominal wall, but the greater omentum and, if the cecum be empty, some coils of small intestine may lie in front of it.
As a rule, it is entirely enveloped by peritoneum, but in a certain number of cases (5 per cent., Berry) the peritoneal covering is not complete, so that the upper part of the posterior surface is uncovered and connected to the iliac fascia by connective tissue. The cecum lies quite free in the abdominal cavity and enjoys a considerable amount of movement, so that it may become herniated down the right inguinal canal, and has occasionally been found in an inguinal hernia on the left side.
The cecum varies in shape, but, according to Treves, in man it may be classified under one of four types. In early fetal life it is short, conical, and broad at the base, with its apex turned upward and medialward toward the ileocolic junction. It then resembles the cecum of some monkeys, e. g mangabey monkey. As the fetus grows the cecum increases in length more than in breadth, so that it forms a longer tube than in the primitive form and without the broad base, but with the same inclination of the apex toward the ileocolic junction. This form is seen in other monkeys, e. g the spider monkey.
As development goes on, the lower part of the tube ceases to grow and the upper part becomes greatly increased, so that at birth there is a narrow tube, the vermiform process, hanging from a conical projection, the cecum. This is the infantile form, and as it persists throughout life in about 2 per cent. of cases, it is regarded by Treves as the first of his four types of human ceca.
The cecum is conical and the appendix rises from its apex. The three longitudinal bands start from the appendix and are equidistant from each other. In the second type, the conical cecum has become quadrate by the growing out of a saccule on either side of the anterior longitudinal band. These saccules are of equal size, and the appendix arises from between them, instead of from the apex of a cone. This type is found in about 3 per cent. of cases.
The third type is the normal type of man. Here the two saccules, which in the second type were uniform, have grown at unequal rates: the right with greater rapidity than the left. In consequence of this an apparently new apex has been formed by the growing downward of the right saccule, and the original apex, with the appendix attached, is pushed over to the left toward the ileocolic junction. The three longitudinal bands still start from the base of the vermiform process, but they are now no longer equidistant from each other, because the right saccule has grown between the anterior and posterolateral bands, pushing them over to the left. This type occurs in about 90 per cent. of cases.
The fourth type is merely an exaggerated condition of the third; the right saccule is still larger, and at the same time the left saccule has become atrophied, so that the original apex of the cecum, with the vermiform process, is close to the ileocolic junction, and the anterior band courses medialward to the same situation. This type is present in about 4 per cent. of cases.
The Vermiform Process[edit | edit source]
The Vermiform Process or Appendix (processus vermiformis) (Fig. 1073) is a long, narrow, worm-shaped tube, which starts from what was originally the apex of the cecum, and may pass in one of several directions: upward behind the cecum; to the left behind the ileum and mesentery; or downward into the lesser pelvis. It varies from 2 to 20 cm. in length, its average being about 8.3 cm. It is retained in position by a fold of peritoneum (mesenteriole), derived from the left leaf of the mesentery.
This fold, in the majority of cases, is more or less triangular in shape, and as a rule extends along the entire length of the tube. Between its two layers and close to its free margin lies the appendicular artery (Fig. 1073). The canal of the vermiform process is small, extends throughout the whole length of the tube, and communicates with the cecum by an orifice which is placed below and behind the ileocecal opening. It is sometimes guarded by a semilunar valve formed by a fold of mucous membrane, but this is by no means constant.
Structure The coats of the vermiform process are the same as those of the intestine: serous, muscular, submucous, and mucous. The serous coat forms a complete investment for the tube, except along the narrow line of attachment of its mesenteriole in its proximal two-thirds. The longitudinal muscular fibers do not form three bands as in the greater part of the large intestine, but invest the whole organ, except at one or two points where both the longitudinal and circular fibers are deficient so that the peritoneal and submucous coats are contiguous over small areas. The circular muscle fibers form a much thicker layer than the longitudinal fibers, and are separated from them by a small amount of connective tissue. The submucous coat is well marked, and contains a large number of masses of lymphoid tissue which cause the mucous membrane to bulge into the lumen and so render the latter of small size and irregular shape. The mucous membrane is lined by columnar epithelium and resembles that of the rest of the large intestine, but the intestinal glands are fewer in number (Fig. 1074).
The Colic Valve[edit | edit source]
(valvula coli; ileocecal valve) (Fig. 1075) The lower end of the ileum ends by opening into the medial and back part of the large intestine, at the point of junction of the cecum with the colon. The opening is guarded by a valve, consisting of two segments or lips, which project into the lumen of the large intestine. If the intestine has been inflated and dried, the lips are of a semilunar shape.
The upper one, nearly horizontal in direction, is attached by its convex border to the line of junction of the ileum with the colon; the lower lip, which is longer and more concave, is attached to the line of junction of the ileum with the cecum. At the ends of the aperture the two segments of the valve coalesce, and are continued as narrow membranous ridges around the canal for a short distance, forming the frenula of the valve The left or anterior end of the aperture is rounded; the right or posterior is narrow and pointed. In the fresh condition, or in specimens which have been hardened in situ the lips project as thick cushion-like folds into the lumen of the large gut, while the opening between them may present the appearance of a slit or may be somewhat oval in shape.
Each lip of the valve is formed by a reduplication of the mucous membrane and of the circular muscular fibers of the intestine, the longitudinal fibers and peritoneum being continued uninterruptedly from the small to the large intestine. The surfaces of the valve directed toward the ileum are covered with villi, and present the characteristic structure of the mucous membrane of the small intestine; while those turned toward the large intestine are destitute of villi, and marked with the orifices of the numerous tubular glands peculiar to the mucous membrane of the large intestine. These differences in structure continue as far as the free margins of the valve. It is generally maintained that this valve prevents reflux from the cecum into the ileum, but in all probability it acts as a sphincter around the end of the ileum and prevents the contents of the ileum from passing too quickly into the cecum.
The Colon[edit | edit source]
The Colon is divided into four parts: the ascending, transverse, descending and sigmoid
The Ascending Colon[edit | edit source]
The Ascending Colon (colon ascendens) is smaller in caliber than the cecum, with which it is continuous. It passes upward, from its commencement at the cecum, opposite the colic valve, to the under surface of the right lobe of the liver, on the right of the gall-bladder, where it is lodged in a shallow depression, the colic impression here it bends abruptly forward and to the left, forming the right colic (hepatic) flexure (Fig. 1056). It is retained in contact with the posterior wall of the abdomen by the peritoneum, which covers its anterior surface and sides, its posterior surface being connected by loose areolar tissue with the Iliacus, Quadratus lumborum, aponeurotic origin of Transversus abdominis, and with the front of the lower and lateral part of the right kidney. Sometimes the peritoneum completely invests it, and forms a distinct but narrow mesocolon. 169 It is in relation, in front, with the convolutions of the ileum and the abdominal parietes.
The Transverse Colon[edit | edit source]
The Transverse Colon (colon transversum) the longest and most movable part of the colon, passes with a downward convexity from the right hypochondriac region across the abdomen, opposite the confines of the epigastric and umbilical zones, into the left hypochondriac region, where it curves sharply on itself beneath the lower end of the spleen, forming the left colic (splenic) flexure In its course it describes an arch, the concavity of which is directed backward and a little upward; toward its splenic end there is often an abrupt U-shaped curve which may descend lower than the main curve.
It is almost completely invested by peritoneum, and is connected to the inferior border of the pancreas by a large and wide duplicature of that membrane, the transverse mesocolon It is in relation, by its upper surface, with the liver and gall-bladder, the greater curvature of the stomach, and the lower end of the spleen; by its under surface, with the small intestine; by its anterior surface, with the anterior layers of the greater omentum and the abdominal parietes; its posterior surface is in relation from right to left with the descending portion of the duodenum, the head of the pancreas, and some of the convolutions of the jejunum and ileum.
The left colic or splenic flexure (Fig. 1056) is situated at the junction of the transverse and descending parts of the colon, and is in relation with the lower end of the spleen and the tail of the pancreas; the flexure is so acute that the end of the transverse colon usually lies in contact with the front of the descending colon. It lies at a higher level than, and on a plane posterior to, the right colic flexure, and is attached to the diaphragm, opposite the tenth and eleventh ribs, by a peritoneal fold, named the phrenicocolic ligament which assists in supporting the lower end of the spleen (see page 1158).
The Descending Colon[edit | edit source]
The Descending Colon (colon descendens) passes downward through the left hypochondriac and lumbar regions along the lateral border of the left kidney. At the lower end of the kidney it turns medialward toward the lateral border of the Psoas, and then descends, in the angle between Psoas and Quadratus lumborum, to the crest of the ilium, where it ends in the iliac colon. The peritoneum covers its anterior surface and sides, while its posterior surface is connected by areolar tissue with the lower and lateral part of the left kidney, the aponeurotic origin of the Transversus abdominis, and the Quadratus lumborum (Fig. 1056). It is smaller in caliber and more deeply placed than the ascending colon, and is more frequently covered with peritoneum on its posterior surface than the ascending colon (Treves). In front of it are some coils of small intestine. The Iliac Colon (Fig. 1076) is situated in the left iliac fossa, and is about 12 to 15 cm. long. It begins at the level of the iliac crest, where it is continuous with the descending colon, and ends in the sigmoid colon at the superior aperture of the lesser pelvis. It curves downward and medialward in front of the Iliacus and Psoas, and, as a rule, is covered by peritoneum on its sides and anterior surface only.
The Sigmoid Colon[edit | edit source]
The Sigmoid Colon (colon sigmoideum; pelvic colon; sigmoid flexure) (Fig. 1076) forms a loop which averages about 40 cm. in length, and normally lies within the pelvis, but on account of its freedom of movement it is liable to be displaced into the abdominal cavity. It begins at the superior aperture of the lesser pelvis, where it is continuous with the iliac colon, and passes transversely across the front of the sacrum to the right side of the pelvis; it then curves on itself and turns toward the left to reach the middle line at the level of the third piece of the sacrum, where it bends downward and ends in the rectum. It is completely surrounded by peritoneum, which forms a mesentery (sigmoid mesocolon), which diminishes in length from the center toward the ends of the loop, where it disappears, so that the loop is fixed at its junctions with the iliac colon and rectum, but enjoys a considerable range of movement in its central portion. Behind the sigmoid colon are the external iliac vessels, the left Piriformis, and left sacral plexus of nerves; in front it is separated from the bladder in the male, and the uterus in the female, by some coils of the small intestine.
The Rectum[edit | edit source]
The Rectum (intestinum rectum) (Fig. 1077) is continuous above with the sigmoid colon, while below it ends in the anal canal. From its origin at the level of the third sacral vertebra it passes downward, lying in the sacrococcygeal curve, and extends for about 2.5 cm. in front of, and a little below, the tip of the coccyx, as far as the apex of the prostate. It then bends sharply backward into the anal canal. It therefore presents two antero-posterior curves: an upper, with its convexity backward, and a lower, with its convexity forward. Two lateral curves are also described, one to the right opposite the junction of the third and fourth sacral vertebrae, and the other to the left, opposite the left sacrococcygeal articulation; they are, however, of little importance.
The rectum is about 12 cm. long, and at its commencement its caliber is similar to that of the sigmoid colon, but near its termination it is dilated to form the rectal ampulla The rectum has no sacculations comparable to those of the colon, but when the lower part of the rectum is contracted, its mucous membrane is thrown into a number of folds, which are longitudinal in direction and are effaced by the distension of the gut.
Besides these there are certain permanent transverse folds, of a semilunar shape, known as Houston’s valves (Fig. 1078). They are usually three in number; sometimes a fourth is found, and occasionally only two are present. One is situated near the commencement of the rectum, on the right side; a second extends inward from the left side of the tube, opposite the middle of the sacrum; a third, the largest and most constant, projects backward from the forepart of the rectum, opposite the fundus of the urinary bladder. When a fourth is present, it is situated nearly 2.5 cm. above the anus on the left and posterior wall of the tube. These folds are about 12 mm. in width, and contain some of the circular fibers of the gut.
In the empty state of the intestine they overlap each other, as Houston remarks, so effectually as to require considerable maneuvering to conduct a bougie or the finger along the canal. Their use seems to be, “to support the weight of fecal matter, and prevent its urging toward the anus, where its presence always excites a sensation demanding its discharge. The peritoneum is related to the upper two-thirds of the rectum, covering at first its front and sides, but lower down its front only; from the latter it is reflected on to the seminal vesicles in the male and the posterior vaginal wall in the female.
The level at which the peritoneum leaves the anterior wall of the rectum to be reflected on to the viscus in front of it is of considerable importance from a surgical point of view, in connection with the removal of the lower part of the rectum. It is higher in the male than in the female. In the former the height of the rectovesical excavation is about 7.5 cm., i. e the height to which an ordinary index finger can reach from the anus. In the female the height of the rectouterine excavation is about 5.5 cm. from the anal orifice. The rectum is surrounded by a dense tube of fascia derived from the fascia endopelvina, but fused behind with the fascia covering the sacrum and coccyx. The facial tube is loosely attached to the rectal wall by areolar tissue in order to allow of distension of the viscus.
Relations of the Rectum[edit | edit source]
The upper part of the rectum is in relation, behind with the superior hemorrhoidal vessels, the left Piriformis, and left sacral plexus of nerves, which separate it from the pelvic surfaces of the sacral vertebrae; in its lower part it lies directly on the sacrum, coccyx, and Levatores ani, a dense fascia alone intervening; in front it is separated above, in the male, from the fundus of the bladder; in the female, from the intestinal surface of the uterus and its appendages, by some convolutions of the small intestine, and frequently by the sigmoid colon; below it is in relation in the male with the triangular portion of the fundus of the bladder, the vesiculae seminales, and ductus deferentes, and more anteriorly with the posterior surface of the prostate; in the female, with the posterior wall of the vagina.
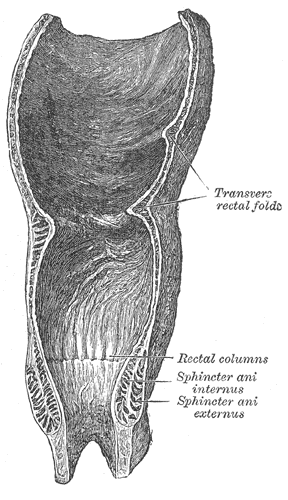
The Anal Canal[edit | edit source]
The Anal Canal (pars analis recti) (Figs. 1079, 1080, 1081), or terminal portion of the large intestine, begins at the level of the apex of the prostate, is directed downward and backward, and ends at the anus. It forms an angle with the lower part of the rectum, and measures from 2.5 to 4 cm. in length. It has no peritoneal covering, but is invested by the Sphincter ani internus, supported by the Levatores ani, and surrounded at its termination by the Sphincter ani externus. In the empty condition it presents the appearance of an antero-posterior longitudinal slit. Behind it is a mass of muscular and fibrous tissue, the anococcygeal body (Symington); in front of it, in the male, but separated by connective tissue from it, are the membranous portion and bulb of the urethra, and the fascia of the urogenital diaphragm; and in the female it is separated from the lower end of the vagina by a mass of muscular and fibrous tissue, named the perineal body
The lumen of the anal canal presents, in its upper half, a number of vertical folds, produced by an infolding of the mucous membrane and some of the muscular tissue. They are known as the rectal columnsMorgagni(Fig. 1078), and are separated from one another by furrows (rectal sinuses), which end below in small valve-like folds, termed anal valves which join together the lower ends of the rectal columns.
Structure[edit | edit source]
The large intestine has four coats: serous, muscular, areolar and mucous The serous coat (tunica serosa) is derived from the peritoneum, and invests the different portions of the large intestine to a variable extent. The cecum is completely covered by the serous membrane, except in about 5 per cent. of cases where the upper part of the posterior surface is uncovered. The ascending, descending, and iliac parts of the colon are usually covered only in front and at the sides; a variable amount of the posterior surface is uncovered. 172 The transverse colon is almost completely invested, the parts corresponding to the attachment of the greater omentum and transverse mesocolon being alone excepted. The sigmoid colon is entirely surrounded. The rectum is covered above on its anterior surface and sides; below, on its anterior aspect only; the anal canal is entirely devoid of any serous covering. In the course of the colon the peritoneal coat is thrown into a number of small pouches filled with fat, called appendices epiploicae They are most numerous on the transverse colon.
The muscular coat (tunica muscularis) consists of an external longitudinal, and an internal circular, layer of non-striped muscular fibers: The longitudinal fibers do not form a continuous layer over the whole surface of the large intestine. In the cecum and colon they are especially collected into three flat longitudinal bands (taenaei coli), each of about 12 mm. in width; one, the posterior, is placed along the attached border of the intestine; the anterior, the largest, corresponds along the arch of the colon to the attachment of the greater omentum, but is in front in the ascending, descending, and iliac parts of the colon, and in the sigmoid colon; the third, or lateral band, is found on the medial side of the ascending and descending parts of the colon, and on the under aspect of the transverse colon. These bands are shorter than the other coats of the intestine, and serve to produce the sacculi which are characteristic of the cecum and colon; accordingly, when they are dissected off, the tube can be lengthened, and its sacculated character disappears. In the sigmoid colon the longitudinal fibers become more scattered; and around the rectum they spread out and form a layer, which completely encircles this portion of the gut, but is thicker on the anterior and posterior surfaces, where it forms two bands, than on the lateral surfaces. In addition, two bands of plain muscular tissue arise from the second and third coccygeal vertebrae, and pass downward and forward to blend with the longitudinal muscular fibers on the posterior wall of the anal canal. These are known as the Rectococcygeal muscles
The circular fibers form a thin layer over the cecum and colon, being especially accumulated in the intervals between the sacculi; in the rectum they form a thick layer, and in the anal canal they become numerous, and constitute the Sphincter ani internus.
The areolar coat (tela submucosa; submucous coat) connects the muscular and mucous layers closely together.
The mucous membrane[edit | edit source]
The mucous membrane (tunica mucosa) in the cecum and colon, is pale, smooth, destitute of villi, and raised into numerous crescentic folds which correspond to the intervals between the sacculi. In the rectum it is thicker, of a darker color, more vascular, and connected loosely to the muscular coat, as in the esophagus.
As in the small intestine, the mucous membrane (Fig. 1082) consists of a muscular layer, the muscularis mucosae; a quantity of retiform tissue in which the vessels ramify; a basement membrane and epithelium which is of the columnar variety, and resembles the epithelium found in the small intestine. The mucous membrane of the large intestine presents for examination glands and solitary lymphatic nodules.
The glands of the great intestine are minute tubular prolongations of the mucous membrane arranged perpendicularly, side by side, over its entire surface; they are longer, more numerous, and placed in much closer apposition than those of the small intestine; and they open by minute rounded orifices upon the surface, giving it a cribriform appearance. Each gland is lined by short columnar epithelium and contains numerous goblet cells.
The solitary lymphatic nodules (noduli lymphatic solitarii) (Fig. 1082) of the large intestine are most abundant in the cecum and vermiform process, but are irregularly scattered also over the rest of the intestine. They are similar to those of the small intestine.
Vessels and Nerves[edit | edit source]
The arteries supplying the colon are derived from the colic and sigmoid branches of the mesenteric arteries. They give off large branches, which ramify between and supply the muscular coats, and after dividing into small vessels in the submucous tissue, pass to the mucous membrane. The rectum is supplied by the superior hemorrhoidal branch of the inferior mesenteric, and the anal canal by the middle hemorrhoidal from the hypogastric, and the inferior hemorrhoidal from the internal pudendal artery. The superior hemorrhoidal, the continuation of the inferior mesenteric, divides into two branches, which run down either side of the rectum to within about 12.5 cm. of the anus; they here split up into about six branches which pierce the muscular coat and descend between it and the mucous membrane in a longitudinal direction, parallel with each other as far as the Sphincter ani internus, where they anastomose with the other hemorrhoidal arteries and form a series of loops around the anus.
The veins of the rectum commence in a plexus of vessels which surrounds the anal canal. In the vessels forming this plexus are smaller saccular dilatations just within the margin of the anus; from the plexus about six vessels of considerable size are given off. These ascend between the muscular and mucous coats for about 12.5 cm., running parallel to each other; they then pierce the muscular coat, and, by their union, form a single trunk, the superior hemorrhoidal vein. This arrangement is termed the hemorrhoidal plexus it communicates with the tributaries of the middle and inferior hemorrhoidal veins, at its commencement, and thus a communication is established between the systemic and portal circulations. The lymphatics of the large intestine are described on page 711.
The nerves are derived from the sympathetic plexuses around the branches of the superior and inferior mesenteric arteries. They are distributed in a similar way to those found in the small intestine. 32
Congenital Hernia—There are some varieties of oblique inguinal hernia (Fig. 1084) depending upon congenital defects in the saccus vaginalis, the pouch of peritoneum which precedes the descent of the testis. Normally this pouch is closed before birth, closure commencing at two points, viz., at the abdominal inguinal ring and at the top of the epididymis, and gradually extending until the whole of the intervening portion is converted into a fibrous cord. From failure in the completion of this process, variations in the relation of the hernial protrusion to the testis and tunica vaginalis are produced; these constitute distinct varieties of inguinal hernia, viz., the hernia of the funicular process and the complete congenital variety.
Where the saccus vaginalis remains patent throughout, the cavity of the tunica vaginalis communicates directly with that of the peritoneum. The intestine descends along this pouch into the cavity of the tunica vaginalis which constitutes the sac of the hernia, and the gut lies in contact with the testis. Though this form of hernia is termed complete congenital the term does not imply that the hernia existed at birth, but merely that a condition is present which may allow of the descent of the hernia at any moment. As a matter of fact, congenital herniae frequently do not appear until adult life. Where the processus vaginalis is occluded at the lower point only, i.e just above the testis, the intestine descends into the pouch of peritoneum as far as the testis, but is prevented from entering the sac of the tunica vaginalis by the septum which has formed between it and the pouch. This is known as hernia into the funicular process or incomplete congenital hernia it differs from the former in that instead of enveloping the testis it lies above it.
Note 169 Treves states that, after a careful examination of one hundred subjects, he found that in fifty-two there was neither an ascending nor a descending mesocolon. In twenty-two there was a descending mesocolon, but no trace of a corresponding fold on the other side. In fourteen subjects there was a mesocolon to both the ascending and the descending segments of the bowel; while in the remaining twelve there was an ascending mesocolon, but no corresponding fold on the left side. It follows, therefore, that in performing lumbar colotomy a mesocolon may be expected upon the left side in 36 per cent. of all cases, and on the right in 26 per cent.—The Anatomy of the Intestinal Canal and Peritoneum in Man, 1885, p. 55.
Note 170 In the Basle nomenclature the descending colon is the portion between the left colic flexure and the superior aperture of the lesser pelvis; it is, however, convenient to describe its lowest part as the iliac colon.
Note 171 Paterson (“The Form of the Rectum,” Journal of Anatomy and Physiology, vol. xliii) utilizes the third fold for the purpose of dividing the rectum into an upper and a lower portion; he considers the latter “to be just as much a duct as the narrower anal canal below,” and maintains that, under normal conditions, it does not contain feces except during the act of defecation.
Note 172 See footnote, p. 1183.
Additional images[edit | edit source]
External links[edit | edit source]
- 09-118h. at Merck Manual of Diagnosis and Therapy Home Edition
| Anatomy of the gastrointestinal tract, excluding the mouth | ||||||
|---|---|---|---|---|---|---|
|
Gray's Anatomy[edit source]
- Gray's Anatomy Contents
- Gray's Anatomy Subject Index
- About Classic Gray's Anatomy
- Glossary of anatomy terms
Anatomy atlases (external)[edit source]
[1] - Anatomy Atlases
| This article is a medical stub. You can help WikiMD by expanding it! | |
|---|---|
| Human systems and organs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Deepika vegiraju, Prab R. Tumpati, MD