The Spinal Nerves
Anatomy > Gray's Anatomy of the Human Body > IX. Neurology > 6. The Spinal Nerves
Henry Gray (1821–1865). Anatomy of the Human Body. 1918.
The Spinal Nerves[edit | edit source]
(Nervi Spinales)
The spinal nerves spring from the medulla spinalis, and are transmitted through the intervertebral foramina. They number thirty-one pairs, which are grouped as follows: Cervical, 8; Thoracic, 12; Lumbar, 5; Sacral, 5; Coccygeal, 1.
cervical nerves[edit | edit source]
The first cervical nerve emerges from the vertebral canal between the occipital bone and the atlas, and is therefore called the suboccipital nerve the eighth issues between the seventh cervical and first thoracic vertebrae.
Nerve Roots Each nerve is attached to the medulla spinalis by two roots, an anterior or ventral and a posterior or dorsal the latter being characterized by the presence of a ganglion, the spinal ganglion
The Anterior Root (radix anterior; ventral root) emerges from the anterior surface of the medulla spinalis as a number of rootlets or filaments (fila radicularia), which coalesce to form two bundles near the intervertebral foramen.
The Posterior Root (radix posterior; dorsal root) is larger than the anterior owing to the greater size and number of its rootlets; these are attached along the posterolateral furrow of the medulla spinalis and unite to form two bundles which join the spinal ganglion. The posterior root of the first cervical nerve is exceptional in that it is smaller than the anterior; it is occasionally wanting.
Spinal Ganglia[edit | edit source]
The Spinal Ganglia (ganglion spinale) are collections of nerve cells on the posterior roots of the spinal nerves. Each ganglion is oval in shape, reddish in color, and its size bears a proportion to that of the nerve root on which it is situated; it is bifid medially where it is joined by the two bundles of the posterior nerve root. The ganglia are usually placed in the intervertebral foramina, immediately outside the points where the nerve roots perforate the dura mater, but there are exceptions to this rule; thus the ganglia of the first and second cervical nerves lie on the vertebral arches of the atlas and axis respectively, those of the sacral nerves are inside the vertebral canal, while that on the posterior root of the coccygeal nerve is placed within the sheath of dura mater.
Structure (Fig. 638)[edit | edit source]
The ganglia consist chiefly of unipolar nerve cells, and from these the fibers of the posterior root take origin—the single process of each cell dividing after a short course into a central fiber which enters the medulla spinalis and a peripheral fiber which runs into the spinal nerve. Two other forms of cells are, however, present, viz.: ('a') the cells of Dogiel, whose axons ramify close to the cell (type II, of Golgi), and are distributed entirely within the ganglion; and ('b') multipolar cells similar to those found in the sympathetic ganglia.
The ganglia of the first cervical nerve may be absent, while small aberrant ganglia consisting of groups of nerve cells are sometimes found on the posterior roots between the spinal ganglia and the medulla spinalis. Each nerve root receives a covering from the pia mater, and is loosely invested by the arachnoid, the latter being prolonged as far as the points where the roots pierce the dura mater. The two roots pierce the dura mater separately, each receiving a sheath from this membrane; where the roots join to form the spinal nerve this sheath is continuous with the epineurium of the nerve.
Size and Direction[edit | edit source]
The roots of the upper four cervical nerves are small, those of the lower four are large. The posterior roots of the cervical nerves bear a proportion to the anterior of three to one, which is greater than in the other regions; their individual filaments are also larger than those of the anterior roots. The posterior root of the first cervical is an exception to this rule, being smaller than the anterior root; in eight per cent. of cases it is wanting. The roots of the first and second cervical nerves are short, and run nearly horizontally to their points of exit from the vertebral canal. From the second to the eighth cervical they are directed obliquely downward, the obliquity and length of the roots successively increasing; the distance, however, between the level of attachment of any of these roots to the medulla spinalis and the points of exit of the corresponding nerves never exceeds the depth of one vertebra.
Thoracic nerves[edit | edit source]
The roots of the thoracic nerves, with the exception of the first, are of small size, and the posterior only slightly exceed the anterior in thickness. They increase successively in length, from above downward, and in the lower part of the thoracic region descend in contact with the medulla spinalis for a distance equal to the height of at least two vertebrae before they emerge from the vertebral canal.
Lumbar,sacral,coccygeal nerves[edit | edit source]
The roots of the lower lumbar and upper sacral nerves are the largest, and their individual filaments the most numerous of all the spinal nerves, while the roots of the coccygeal nerve are the smallest. The roots of the lumbar, sacral, and coccygeal nerves run vertically downward to their respective exits, and as the medulla spinalis ends near the lower border of the first lumbar vertebra it follows that the length of the successive roots must rapidly increase. As already mentioned (page 750), the term cauda equina is applied to this collection of nerve roots.
From the description given it will be seen that the largest nerve roots, and consequently the largest spinal nerves, are attached to the cervical and lumbar swellings of the medulla spinalis; these nerves are distributed to the upper and lower limbs.
Connections with Sympathetic[edit | edit source]
Immediately beyond the spinal ganglion, the anterior and posterior nerve roots unite to form the spinal nerve which emerges through the intervertebral foramen. Each spinal nerve receives a branch (gray ramus communicans) from the adjacent ganglion of the sympathetic trunk, while the thoracic, and the first and second lumbar nerves each contribute a branch (white ramus communicans) to the adjoining sympathetic ganglion. The second, third, and fourth sacral nerves also supply white rami; these, however, are not connected with the ganglia of the sympathetic trunk, but run directly into the pelvic plexuses of the sympathetic.
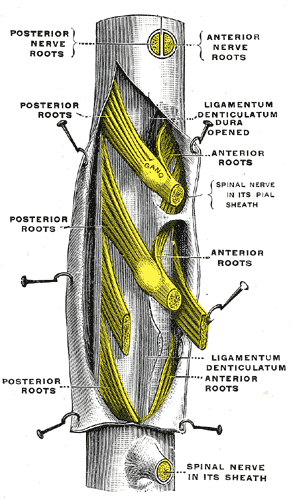
The spinal cord with dura cut open, showing the exits of the spinal nerves.
Structure[edit | edit source]
Each typical spinal nerve contains fibers belonging to two systems, viz., the somatic and the sympathetic or splanchnic as well as fibers connecting these systems with each other (Fig. 799).
1.The somatic fibers[edit | edit source]
The somatic fibers are efferent and afferent. The efferent fibers originate in the cells of the anterior column of the medulla spinalis, and run outward through the anterior nerve roots to the spinal nerve. They convey impulses to the voluntary muscles, and are continuous from their origin to their peripheral distribution. The afferent fibers convey impressions inward from the skin, etc., and originate in the unipolar nerve cells of the spinal ganglia. The single processes of these cells divide into peripheral and central fibers, and the latter enter the medulla spinalis through the posterior nerve roots.
2. The sympathetic fibers[edit | edit source]
The sympathetic fibers are also efferent and afferent. The efferent fibers, preganglionic fibers, originate in the lateral column of the medulla spinalis, and are conveyed through the anterior nerve root and the white ramus communicans to the corresponding ganglion of the sympathetic trunk; here they may end by forming synapses around its cells, or may run through the ganglion to end in another of the ganglia of the sympathetic trunk, or in a more distally placed ganglion in one of the sympathetic plexuses. In all cases they end by forming synapses around other nerve cells. From the cells of the ganglia of the sympathetic trunk other fibers, postganglionic fibers, take origin; some of these run through the gray rami communicantes to join the spinal nerves, along which they are carried to the bloodvessels of the trunk and limbs, while others pass to the viscera, either directly or after interruption in one of the distal ganglia. The afferent fibers are derived partly from the unipolar cells and partly from the multipolar cells of the spinal ganglia. Their peripheral processes are carred through the white rami communicantes, and after passing through one or more sympathetic ganglia (but always without interruption in them) finally end in the tissues of the viscera. The central processes of the unipolar cells enter the medulla spinalis through the posterior nerve root and form synapses around either somatic or sympathetic efferent neurons, thus completing reflex arcs. The dendrites of the multipolar nerve cells form synapses around the cells of type II (cells of Dogiel) in the spinal ganglia, and by this path the original impulse is transferred from the sympathetic to the somatic system, through which it is conveyed to the sensorium.
Divisions[edit | edit source]
After emerging from the intervertebral foramen, each spinal nerve gives off a small meningeal branch which reënters the vertebral canal through the intervertebral foramen and supplies the vertebrae and their ligaments, and the bloodvessels of the medulla spinalis and its membranes. The spinal nerve then splits into a posterior or dorsal and an anterior or ventral division each receiving fibres from both nerve roots.
Function[edit | edit source]
| Level | Motor function |
|---|---|
| C1–C6 | Neck flexors |
| C1–T1 | Neck extensors |
| C3, C4, C5 | Supply diaphragm (mostly C4) |
| C5, C6 | Move shoulder, raise arm (deltoid); flex elbow (biceps) |
| C6 | externally rotate (supinate) the arm |
| C6, C7 | Extend elbow and wrist (triceps and wrist extensors); pronate wrist |
| C7, C8 | Flex wrist; supply small muscles of the hand |
| T1–T6 | Intercostals and trunk above the waist |
| T7–L1 | Abdominal muscles |
| L1–L4 | Flex hip joint |
| L2, L3, L4 | Adduct thigh; Extend leg at the knee (quadriceps femoris) |
| L4, L5, S1 | abduct thigh; Flex leg at the knee (hamstrings); Dorsiflex foot (tibialis anterior); Extend toes |
| L5, S1, S2 | Extend leg at the hip (gluteus maximus); flex foot and flex toes |
Additional Images[edit | edit source]
- Dissection images
Gray's Anatomy[edit source]
- Gray's Anatomy Contents
- Gray's Anatomy Subject Index
- About Classic Gray's Anatomy
- Glossary of anatomy terms
Anatomy atlases (external)[edit source]
[1] - Anatomy Atlases
| This article is a medical stub. You can help WikiMD by expanding it! | |
|---|---|
| Human systems and organs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Deepika vegiraju, Prab R. Tumpati, MD