The Spinal Cord or Medulla Spinalis
Anatomy > Gray's Anatomy of the Human Body > IX. Neurology > 3. The Spinal Cord or Medulla Spinalis
Henry Gray (1821–1865). Anatomy of the Human Body. 1918.
The Spinal Cord or Medulla Spinalis[edit | edit source]
The medulla spinalis or spinal cord forms the elongated, nearly cylindrical, part of the central nervous system which occupies the upper two-thirds of the vertebral canal. Its average length in the male is about 45 cm., in the female from 42 to 43 cm., while its weight amounts to about 30 gms. It extends from the level of the upper border of the atlas to that of the lower border of the first, or upper border of the second, lumbar vertebra. Above, it is continuous with the brain; below, it ends in a conical extremity, the conus medullaris from the apex of which a delicate filament, the filum terminale descends as far as the first segment of the coccyx (Fig. 661).
The position of the medulla spinalis varies with the movements of the vertebral column, its lower extremity being drawn slightly upward when the column is flexed. It also varies at different periods of life; up to the third month of fetal life the medulla spinalis is as long as the vertebral canal, but from this stage onward the vertebral column elongates more rapidly than the medulla spinalis, so that by the end of the fifth month the medulla spinalis terminates at the base of the sacrum, and at birth about the third lumbar vertebra.
The medulla spinalis does not fill the part of the vertebral canal in which it lies; it is ensheathed by three protective membranes, separated from each other by two concentric spaces. The three membranes are named from without inward, the dura mater the arachnoid and the pia mater
The dura mater is a strong, fibrous membrane which forms a wide, tubular sheath; this sheath extends below the termination of the medulla spinalis and ends in a pointed cul-de-sac at the level of the lower border of the second sacral vertebra. The dura mater is separated from the wall of the vertebral canal by the epidural cavity which contains a quantity of loose areolar tissue and a plexus of veins; between the dura mater and the subjacent arachnoid is a capillary interval, the subdural cavity which contains a small quantity of fluid, probably of the nature of lymph.
The arachnoid is a thin, transparent sheath, separated from the pia mater by a comparatively wide interval, the subarachnoid cavity which is filled with cerebrospinal fluid.
The pia mater closely invests the medulla spinalis and sends delicate septa into its substance; a narrow band, the ligamentum denticulatum extends along each of its lateral surfaces and is attached by a series of pointed processes to the inner surface of the dura mater.
Spinal cord segments[edit | edit source]
Thirty-one pairs of spinal nerves spring from the medulla spinalis, each nerve having an anterior or ventral, and a posterior or dorsal root, the latter being distinguished by the presence of an oval swelling, the spinal ganglion which contains numerous nerve cells. Each root consists of several bundles of nerve fibers, and at its attachment extends for some distance along the side of the medulla spinalis.
The pairs of spinal nerves are grouped as follows: cervical 8, thoracic 12, lumbar 5, sacral 5, coccygeal 1, and, for convenience of description, the medulla spinalis is divided into cervical, thoracic, lumbar and sacral regions, corresponding with the attachments of the different groups of nerves.
Although no trace of transverse segmentation is visible on the surface of the medulla spinalis, it is convenient to regard it as being built up of a series of superimposed spinal segments or neuromeres each of which has a length equivalent to the extent of attachment of a pair of spinal nerves. Since the extent of attachment of the successive pairs of nerves varies in different parts, it follows that the spinal segments are of varying lengths; thus, in the cervical region they average about 13 mm., in the mid-thoracic region about 26 mm., while in the lumbar and sacral regions they diminish rapidly from about 15 mm. at the level of the first pair of lumbar nerves to about 4 mm. opposite the attachments of the lower sacral nerves.

As a consequence of the relative inequality in the rates of growth of the medulla spinalis and vertebral column, the nerve roots, which in the early embryo passed transversely outward to reach their respective intervertebral foramina, become more and more oblique in direction from above downward, so that the lumbar and sacral nerves descend almost vertically to reach their points of exit. From the appearance these nerves present at their attachment to the medulla spinalis and from their great length they are collectively termed the cauda equina (Fig. 662).
Filum terminale[edit | edit source]
The filum terminale is a delicate filament, about 20 cm. in length, prolonged downward from the apex of the conus medullaris. It consists of two parts, an upper and a lower.
The upper part, or filum terminale internum measures about 15 cm. in length and reaches as far as the lower border of the second sacral vertebra. It is contained within the tubular sheath of dura mater, and is surrounded by the nerves forming the cauda equina, from which it can be readily recognized by its bluish-white color.
The lower part, or filum terminale externum is closely invested by, and is adherent to, the dura mater; it extends downward from the apex of the tubular sheath and is attached to the back of the first segment of the coccyx. The filum terminale consists mainly of fibrous tissue, continuous above with that of the pia mater. Adhering to its outer surface, however, are a few strands of nerve fibers which probably represent rudimentary second and third coccygeal nerves; further, the central canal of the medulla spinalis extends downward into it for 5 or 6 cm.
Enlargements[edit | edit source]
The medulla spinalis is not quite cylindrical, being slightly flattened from before backward; it also presents two swellings or enlargements, an upper or cervical, and a lower or lumbar (Fig. 663).
cervical enlargement[edit | edit source]
The cervical enlargement is the more pronounced, and corresponds with the attachments of the large nerves which supply the upper limbs. It extends from about the third cervical to the second thoracic vertebra, its maximum circumference (about 38 mm.) being on a level with the attachment of the sixth pair of cervical nerves.
lumbar enlargement[edit | edit source]
The lumbar enlargement gives attachment to the nerves which supply the lower limbs. It commences about the level of the ninth thoracic vertebra, and reaches its maximum circumference, of about 33 mm., opposite the last thoracic vertebra, below which it tapers rapidly into the conus medullaris.
Fissures and Sulci (Fig. 664)[edit | edit source]
An anterior median fissure and a posterior median sulcus incompletely divide the medulla spinalis into two symmetrical parts, which are joined across the middle line by a commissural band of nervous matter.
The Anterior Median Fissure (fissura mediana anterior) has an average depth of about 3 mm., but this is increased in the lower part of the medulla spinalis. It contains a double fold of pia mater, and its floor is formed by a transverse band of white substance, the anterior white commissure which is perforated by bloodvessels on their way to or from the central part of the medulla spinalis.
The Posterior Median Sulcus (sulcus medianus posterior) is very shallow; from it a septum of neuroglia reaches rather more than half-way into the substance of the medulla spinalis; this septum varies in depth from 4 to 6 mm., but diminishes considerably in the lower part of the medulla spinalis.
On either side of the posterior median sulcus, and at a short distance from it, the posterior nerve roots are attached along a vertical furrow named the posterolateral sulcus The portion of the medulla spinalis which lies between this and the posterior median sulcus is named the posterior funiculus
In the cervical and upper thoracic regions this funiculus presents a longitudinal furrow, the postero-intermediate sulcus this marks the position of a septum which extends into the posterior funiculus and subdivides it into two fasciculi—a medial, named the fasciculus gracilis (tract of Goll); and a lateral, the fasciculus cuneatus (tract of Burdach) (Fig. 672).
The portion of the medulla spinalis which lies in front of the posterolateral sulcus is termed the antero-lateral region The anterior nerve roots, unlike the posterior, are not attached in linear series, and their position of exit is not marked by a sulcus. They arise by separate bundles which spring from the anterior column of gray substance and, passing forward through the white substance, emerge over an area of some slight width. The most lateral of these bundles is generally taken as a dividing line which separates the antero-lateral region into two parts, viz., an anterior funiculus between the anterior median fissure and the most lateral of the anterior nerve roots; and a lateral funiculus between the exit of these roots and the postero-lateral sulcus. In the upper part of the cervical region a series of nerve roots passes outward through the lateral funiculus of the medulla spinalis; these unite to form the spinal portion of the accessory nerve, which runs upward and enters the cranial cavity through the foramen magnum.
The Internal Structure of the Medulla Spinalis[edit | edit source]
On examining a transverse section of the medulla spinalis (Fig. 664) it is seen to consist of gray and white nervous substance, the former being enclosed within the latter.
Gray Substance[edit | edit source]
(substantia grisea centralis)
The gray substance consists of two symmetrical portions, one in each half of the medulla spinalis: these are joined across the middle line by a transverse commissure of gray substance, through which runs a minute canal, the central canal just visible to the naked eye. In a transverse section each half of the gray substance is shaped like a comma or crescent, the concavity of which is directed laterally; and these, together with the intervening gray commissure, present the appearance of the letter H.
An imaginary coronal plane through the central canal serves to divide each crescent into an anterior or ventral and a posterior or dorsal column
The Anterior Column (columna anterior; anterior cornu), directed forward, is broad and of a rounded or quadrangular shape. Its posterior part is termed the base, and its anterior part the head but these are not differentiated from each other by any well-defined constriction. It is separated from the surface of the medulla spinalis by a layer of white substance which is traversed by the bundles of the anterior nerve roots. In the thoracic region, the postero-lateral part of the anterior column projects lateralward as a triangular field, which is named the lateral column (columna lateralis; lateral cornu).
The Posterior Column (columna posterior; posterior cornu) is long and slender, and is directed backward and lateralward: it reaches almost as far as the posterolateral sulcus, from which it is separated by a thin layer of white substance, the tract of Lissauer
It consists of a base directly continuous with the base of the anterior horn, and a neck or slightly constricted portion, which is succeeded by an oval or fusiform area, termed the head of which the apex approaches the posterolateral sulcus. The apex is capped by a V-shaped or crescentic mass of translucent, gelatinous neuroglia, termed the substantia gelatinosa of Rolando which contains both neuroglia cells, and small nerve cells. Between the anterior and posterior columns the gray substance extends as a series of processes into the lateral funiculus, to form a net-work called the formatio reticularis
The quantity of gray substance, as well as the form which it presents on transverse section, varies markedly at different levels. In the thoracic region it is small, not only in amount but relatively to the surrounding white substance. In the cervical and lumbar enlargements it is greatly increased: in the latter, and especially in the conus medullaris, its proportion to the white substance is greatest (Fig. 665).
In the cervical region its posterior column is comparatively narrow, while its anterior is broad and expanded; in the thoracic region, both columns are attenuated, and the lateral column is evident; in the lumbar enlargement, both are expanded; while in the conus medullaris the gray substance assumes the form of two oval masses, one in each half of the cord, connected together by a broad gray commissure.
The Central Canal[edit | edit source]
The Central Canal (canalis centralis) runs throughout the entire length of the medulla spinalis. The portion of gray substance in front of the canal is named the anterior gray commissure that behind it, the posterior gray commissure The former is thin, and is in contact anteriorly with the anterior white commissure: it contains a couple of longitudinal veins, one on either side of the middle line. The posterior gray commissure reaches from the central canal to the posterior median septum, and is thinnest in the thoracic region, and thickest in the conus medullaris.
The central canal is continued upward through the lower part of the medulla oblongata, and opens into the fourth ventricle of the brain; below, it reaches for a short distance into the filum terminale. In the lower part of the conus medullaris it exhibits a fusiform dilatation, the terminal ventricle this has a vertical measurement of from 8 to 10 mm., is triangular on cross-section with its base directed forward, and tends to undergo obliteration after the age of forty years.
Throughout the cervical and thoracic regions the central canal is situated in the anterior third of the medulla spinalis; in the lumbar enlargement it is near the middle, and in the conus medullaris it approaches the posterior surface.
It is filled with cerebrospinal fluid, and lined by ciliated, columnar epithelium, outside of which is an encircling band of gelatinous substance, the substantia gelatinosa centralis This gelatinous substance consists mainly of neuroglia, but contains a few nerve cells and fibers; it is traversed by processes from the deep ends of the columnar ciliated cells which line the central canal (Fig. 667).
Structure of the Gray Substance[edit | edit source]
The gray substance consists of numerous nerve cells and nerve fibers held together by neuroglia. Throughout the greater part of the gray substance the neuroglia presents the appearance of a sponge-like network, but around the central canal and on the apices of the posterior columns it consists of the gelatinous substance already referred to.
The nerve cells are multipolar, and vary greatly in size and shape. They consist of
(1) motor cells of large size, which are situated in the anterior horn, and are especially numerous in the cervical and lumbar enlargements; the axons of most of these cells pass out to form the anterior nerve roots, but before leaving the white substance they frequently give off collaterals, which reënter and ramify in the gray substance.
(2) Cells of small or medium size, whose axons pass into the white matter, where some pursue an ascending, and others a descending course, but most of them divide in a T-shape manner into descending and ascending processes. They give off collaterals which enter and ramify in the gray substance, and the terminations of the axons behave in a similar manner.
The lengths of these axons vary greatly: some are short and pass only between adjoining spinal segments, while others are longer and connect more distant segments. These cells and their processes constitute a series of association or intersegmental neurons (Fig. 668), which link together the different parts of the medulla spinalis.
The axons of most of these cells are confined to that side of the medulla spinalis in which the nerve cells are situated, but some cross to the opposite side through the anterior commissure, and are termed crossed commissural fibers Some of these latter end directly in the gray substance, while others enter the white substance, and ascend or descend in it for varying distances, before finally terminating in the gray substance.
(3) Cells of the type II of Golgi, limited for the most part to the posterior column, are found also in the substantia gelatinosa of Rolando; their axons are short and entirely confined to the gray substance, in which they break up into numerous fine filaments. Most of the nerve cells are arranged in longitudinal columns, and appear as groups on transverse section (Figs. 669, 670, 671).
Nerve Cells in the Anterior Column[edit | edit source]
The nerve cells in the anterior column are arranged in columns of varying length. The longest occupies the medial part of the anterior column, and is named the antero-medial column: it is well marked in C4, C5, again from C8 to L4, it disappears in L5 and S1 but is well marked in S2, S3 and S4 (Bruce). 114 Behind it is a dorso-medial column of small cells, which is not represented in L5, S1, S2 nor below S4. Its axons probably pass into the dorsal rami of the spinal nerves to supply the dorsal musculature of the spinal column. In the cervical and lumbar enlargements, where the anterior column is expanded in a lateral direction, the following additional columns are present, viz.: ('a') antero-lateral which consists of two groups, one in C4, C5, C6 the other in C6, C7, C8 in the cervical enlargement and of a group from L2 to S2 in the lumbo-sacral enlargement; ('b') postero-lateral in the lower five cervical, lower four lumbar, and upper three sacral segments; (c) post-postero-lateral in the last cervical, first thoracic, and upper three sacral segments; and (d) a central in the lower four lumbar and upper two sacral segments. These cell groups are evidently related to the nerve roots of the brachial and sacral plexuses and supply fibers to the muscles of the arm and leg. Throughout the base of the anterior column are scattered solitary cells, the axons of some of which form crossed commissural fibers, while others constitute the motor fibers of the posterior nerve roots. (See footnote, page 755.)
Nerve Cells in the Lateral Column[edit | edit source]
These form a column which is best marked where the lateral gray column is differentiated, viz., in the thoracic region; 115 but it can be traced throughout the entire length of the medulla spinalis in the form of groups of small cells which are situated in the anterior part of the formatio reticularis.
In the upper part of the cervical region and lower part of the medulla oblongata as well as in the third and fourth sacral segments this column is again differentiated. In the medulla it is known as the lateral nucleus
The cells of this column are fusiform or star-shaped, and of a medium size: the axons of some of them pass into the anterior nerve roots, by which they are carried to the sympathetic nerves: they constitute the white rami and are sympathetic or visceral efferent fibers; they are also known as preganglionic fibers of the sympathetic system the axons of others pass into the anterior and lateral funiculi, where they become longitudinal.
Nerve Cells in the Posterior Column[edit | edit source]
1. The dorsal nucleus (nucleus dorsalis; column of Clarke) occupies the medial part of the base of the posterior column, and appears on the transverse section as a well-defined oval area. It begins below at the level of the second or third lumbar nerve, and reaches its maximum size opposite the twelfth thoracic nerve. Above the level of the ninth thoracic nerve its size diminishes, and the column ends opposite the last cervical or first thoracic nerve. It is represented, however, in the other regions by scattered cells, which become aggregated to form a cervical nucleus opposite the third cervical nerve, and a sacral nucleus in the middle and lower part of the sacral region. Its cells are of medium size, and of an oval or pyriform shape; their axons pass into the peripheral part of the lateral funiculus of the same side, and there ascend, probably in dorsal spinocerebellar (direct cerebellar) fasciculus
2. The nerve cells in the substantia gelatinosa of Rolando are arranged in three zones: a posterior or marginal, of large angular or fusiform cells; an intermediate, of small fusiform cells; and an anterior, of star-shaped cells. The axons of these cells pass into the lateral and posterior funiculi, and there assume a vertical course. In the anterior zone some Golgi cells are found whose short axons ramify in the gray substance.
3. Solitary cells of varying form and size are scattered throughout the posterior column. Some of these are grouped to form the posterior basal column in the base of the posterior column, lateral to the dorsal nucleus; the posterior basal column is well-marked in the gorilla (Waldeyer), but is ill-defined in man. The axons of its cells pass partly to the posterior and lateral funiculi of the same side, and partly through the anterior white commissure to the lateral funiculus of the opposite side. Golgi cells, type II, located in this region send axons to the lateral and ventral columns.
A few star-shaped or fusiform nerve cells of varying size are found in the substantia gelatinosa centralis. Their axons pass into the lateral funiculus of the same, or of the opposite side.
The nerve fibers in the gray substance form a dense interlacement of minute fibrils among the nerve cells. This interlacement is formed partly of axons which pass from the cells in the gray substance to enter the white funiculi or nerve roots; partly of the axons of Golgi’s cells which ramify only in the gray substance; and partly of collaterals from the nerve fibers in the white funiculi which, as already stated, enter the gray substance and ramify within it.
White Substance (substantia alba)[edit | edit source]
The white substance of the medulla spinalis consists of medullated nerve fibers imbedded in a spongelike net-work of neuroglia, and is arranged in three funiculi: anterior, lateral, and posterior.
The anterior funiculus lies between the anterior median fissure and the most lateral of the anterior nerve roots:
The lateral funiculus between these nerve roots and the postero-lateral sulcus; and the posterior funiculus between the postero-lateral and the posterior median sulci (Fig. 672).
The fibers vary greatly in thickness, the smallest being found in the fasciculus gracilis, the tract of Lissauer and inner part of the lateral funiculus; while the largest are situated in the anterior funiculus, and in the peripheral part of the lateral funiculus.
Some of the nerve fibers assume a more or less transverse direction, as for example those which cross from side to side in the anterior white commissure, but the majority pursue a longitudinal course and are divisible into
(1) those connecting the medulla spinalis with the brain and conveying impulses to or from the latter, and
(2) those which are confined to the medulla spinalis and link together its different segments, i. e intersegmental or association fibers.
Nerve Fasciculi[edit | edit source]
The longitudinal fibers are grouped into more or less definite bundles or fasciculi. These are not recognizable from each other in the normal state, and their existence has been determined by the following methods:
(1) A. Waller discovered that if a bundle of nerve fibers be cut, the portions of the fibers which are separated from their cells rapidly degenerate and become atrophied, while the cells and the parts of the fibers connected with them undergo little alteration.
This is known as Wallerian degeneration Similarly, if a group of nerve cells be destroyed, the fibers arising from them undergo degeneration. Thus, if the motor cells of the cerebral cortex be destroyed, or if the fibers arising from these cells be severed, a descending degeneration from the seat of injury takes place in the fibers. In the same manner, if a spinal ganglion be destroyed, or the fibers which pass from it into the medulla spinalis be cut, an ascending degeneration will extend along these fibers.
(2) Pathological changes, especially in man, have given important information by causing ascending and descending degenerations.
(3) By tracing the development of the nervous system, it has been observed that at first the nerve fibers are merely naked axis-cylinders, and that they do not all acquire their medullary sheaths at the same time; hence the fibers can be grouped into different bundles according to the dates at which they receive their medullary sheaths.
(4) Various methods of staining nervous tissue are of great value in tracing the course and mode of termination of the axis-cylinder processes.
Fasciculi in the Anterior Funiculus. [edit | edit source]
Descending Fasciculi
The anterior cerebrospinal (fasciculus cerebrospinalis anterior; direct pyramidal tract), which is usually small, but varies inversely in size with the lateral cerebrospinal fasciculus. It lies close to the anterior median fissure, and is present only in the upper part of the medulla spinalis; gradually diminishing in size as it descends, it ends about the middle of the thoracic region. It consists of descending fibers which arise from cells in the motor area of the cerebral hemisphere of the same side, and which, as they run downward in the medulla spinalis, cross in succession through the anterior white commissure to the opposite side, where they end, either directly or indirectly, by arborizing around the motor cells in the anterior column. A few of its fibers are said to pass to the lateral column of the same side and to the gray matter at the base of the posterior column. They conduct voluntary motor impulses from the precentral gyrus to the motor centers of the cord.
The vestibulospinal fasciculus situated chiefly in the marginal part of the funiculus and mainly derived from the cells of Deiters’ nucleus, of the same and the opposite side, i. e the chief terminal nucleus of the vestibular nerve. Fibers are also contributed to this fasciculus from scattered cells of the articular formation of the medulla oblongata, the pons and the mid-brain (tegmentum). The other terminal nuclei of the vestibular nerve also contribute fibers. In the brain stem these fibers form part of the median longitudinal bundle. The fasciculus can be traced to the sacral region. Its terminals and collaterals end either directly or indirectly among the motor cells of the anterior column. This fasciculus is probably concerned with equilibratory reflexes.
The tectospinal fasciculus situated partly in the anterior and partly in the lateral funiculus, is mainly derived from the opposite superior colliculus of the mid-brain. The fibers from the superior colliculus cross the median raphé in the fountain decussation of Meynert and descend as the ventral longitudinal bundle in the reticular formation of the brain-stem. Its collaterals and terminals end either directly or indirectly among the motor cells of the anterior column of the same side. Since the superior colliculus is an important visual reflex center, the tectospinal fasciculus is probably concerned with visual reflexes.
Ascending Fasciculi
The ventral spinothalamic fasciculus situated in the marginal part of the funiculus and intermingled more or less with the vestibulo-spinal fasciculus, is derived from cells in the posterior column or intermediate gray matter of the opposite side. Their axons cross in the anterior commissure. This is a somewhat doubtful fasciculus and its fibers are supposed to end in the thalamus and to conduct certain of the touch impulses.
The remaining fibers of the anterior funiculus constitute what is termed the anterior proper fasciculus (fasciculus anterior proprius; anterior basis bundle). It consists of longitudinal intersegmental fibers which arise from cells in the gray substance, more especially from those of the medial group of the anterior column, and, after a longer or shorter course, reënter the gray substance; ('b') fibers which cross in the anterior white commissure from the gray substance of the opposite side.
Fasciculi in the Lateral Funiculus[edit | edit source]
1. Descending Fasciculi
('a') The lateral cerebrospinal fasciculus (fasciculus cerebrospinalis lateralis; crossed pyramidal tract) extends throughout the entire length of the medulla spinalis, and on transverse section appears as an oval area in front of the posterior column and medial to the cerebellospinal. Its fibers arise from cells in the motor area of the cerebral hemisphere of the opposite side. They pass downward in company with those of the anterior cerebrospinal fasciculus through the same side of the brain as that from which they originate, but they cross to the opposite side in the medulla oblongata and descend in the lateral funiculus of the medulla spinalis.
It is probable that the fibers of the anterior and lateral cerebrospinal fasciculi are not related in this direct manner with the cells of the anterior column, but terminate by arborizing around the cells at the base of the posterior column and the cells of Clarke’s column, which in turn link them to the motor cells in the anterior column, usually of several segments of the cord. In consequence of these interposed neurons the fibers of the cerebrospinal fasciculi correspond not to individual muscles, but to associated groups of muscles. The anterior and lateral cerebrospinal fasciculi constitute the motor fasciculi of the medulla spinalis and have their origins in the motor cells of the cerebral cortex. They descend through the internal capsule of the cerebrum, traverse the cerebral peduncles and pons and enter the pyramid of the medulla oblongata. In the lower part of the latter about two-thirds of them cross the middle line and run downward in the lateral funiculus as the lateral cerebrospinal fasciculus, while the remaining fibers do not cross the middle line, but are continued into the same side of the medulla spinalis, where they form the anterior cerebrospinal fasciculus. The fibers of the latter, however, cross the middle line in the anterior white commissure, and thus all the motor fibers from one side of the brain ultimately reach the opposite side of the medulla spinalis. The proportion of fibers which cross in the medulla oblongata is not a constant one, and thus the anterior and lateral cerebrospinal fasciculi vary inversely in size. Sometimes the former is absent, and in such cases it may be presumed that the decussation of the motor fibers in the medulla oblongata has been complete. The fibers of these two fasciculi do not acquire their medullary sheaths until after birth. In some animals the motor fibers are situated in the posterior funiculus.
('b') The rubrospinal fasciculus (Monakow) (prepyramidal tract), lies on the ventral aspect of the lateral cerebrospinal fasciculus and on transverse section appears as a somewhat triangular area. Its fibers descend from the mid-brain, where they have their origin in the red nucleus of the tegmentum of the opposite side. Its terminals and collaterals end either directly or indirectly in relation with the motor cells of the anterior column. The rubrospinal fasciculus is supposed to be concerned with cerebellar reflexes since fibers which pass from the cerebellum through the superior peduncle send many collaterals and terminals to the red nucleus.
(c) The olivospinal fasciculus (Helweg) arises in the vicinity of the inferior olivary nucleus in the medulla oblongata, and is seen only in the cervical region of the medulla spinalis, where it forms a small triangular area at the periphery, close to the most lateral of the anterior nerve roots. Its exact origin and its mode of ending have not yet been definitely made out.
2. Ascending Fasciculi. ('a') The dorsal spinocerebellar fasciculus (fasciculus cerebellospinalis; direct cerebellar tract of Flechsig) is situated at the periphery of the posterior part of the lateral funiculus, and on transverse section appears as a flattened band reaching as far forward as a line drawn transversely through the central canal. Medially, it is in contact with the lateral cerebrospinal fasciculus, behind, with the fasciculus of Lissauer. It begins about the level of the second or third lumbar nerve, and increasing in size as it ascends, passes to the vermis of the cerebellum through the inferior peduncle. Its fibers are generally regarded as being formed by the axons of the cells of the dorsal nucleus (Clarke’s column); they receive their medullary sheaths about the sixth or seventh month of fetal life. Its fibers are supposed to conduct impulses of unconscious muscle sense.
The superficial antero-lateral fasciculus (tract of Gowers) consists of four fasciculi, the ventral spinocerebellar, the lateral spinothalamic, the spinotectal and the ventral spinothalamic.
('b') The ventral spinocerebellar fasciculus (Gowers) skirts the periphery of the lateral funiculus in front of the dorsal spinocerebellar fasciculus. In transverse section it is shaped somewhat like a comma, the expanded end of which lies in front of the dorsal spinocerebellar fasciculus while the tail reaches forward into the anterior funiculus. Its fibers come from the same but mostly from the opposite side of the medulla spinalis and cross both in the anterior white commissure and in the gray commissure; they are probably derived from the cells of the dorsal nucleus and from other cells of the posterior column and the intermediate portion of the gray matter. The ventral spinocerebellar fasciculus begins about the level of the third pair of lumbar nerves, and can be followed into the medulla oblongata and pons almost to the level of the inferior colliculus where it crosses over the superior peduncle and then passes backward along its medial border to reach the vermis of the cerebellum. In the pons it lies along the lateral edge of the lateral lemniscus. Some of its fibers join the dorsal spinocerebellar fasciculus at the level of the inferior peduncle and pass with them into the cerebellum. Other fibers are said to continue upward in the dorso-lateral part of the tegmentum of the mid-brain probably as far as the thalamus.
(c) The lateral spinothalamic fasciculus is supposed to come from cells in the dorsal column and the intermediate gray matter whose axons cross in the anterior commissure to the opposite lateral funiculus where they pass upward on the medial side of the ventral spinocerebellar fasciculus; on reaching the medulla oblongata they continue in the formatio reticularis near the median fillet and probably terminate in the ventro-lateral region of the thalamus. It is supposed to conduct impulses of pain and temperature. The lateral and ventral spinothalamic fasciculi are sometimes termed the secondary sensory fasciculus or spinal lemniscus
(d) The spinotectal fasciculus is supposed to arise in the dorsal column and terminate in the (inferior ?) and superior colliculi. It is situated ventral to the lateral spinothalamic fasciculus, but its fibers are more or less intermingled with it. It is also known as the spino-quadrigeminal system of Mott In the brain-stem the fibers run lateral from the inferior olive, ventro-lateral from the superior olive, then ventro-medial from the spinal tract of the trigeminal; the fibers come to lie in the medial portion of the lateral lemniscus.
(e) The fasciculus of Lissauer is a small strand situated in relation to the tip of the posterior column close to the entrance of the posterior nerve roots. It consists of fine fibers which do not receive their medullary sheaths until toward the close of fetal life. It is usually regarded as being formed by some of the fibers of the posterior nerve roots, which ascend for a short distance in the tract and then enter the posterior column, but since its fibers are myelinated later than those of the posterior nerve roots, and do not undergo degeneration in locomotor ataxia, they are probably intersegmental in character. In addition the fasciculus or tract of Lissauer contains great numbers of fine non-medullated fibers derived mostly from the dorsal roots but partly endogenous in origin. These fibers are intimately related to the substantia gelatinosa which is probably the terminal nucleus. The non-medullated fibers ascend or descend for short distances not exceeding one or two segments, but most of them enter the substantia gelatinosa at or near the level of their origin. Ransom 118 suggests that these non-medullated fibers and the substantia gelatinosa are concerned with the reflexes associated with pain impulses.
(f) The lateral proper fasciculus (fasciculus lateralis proprius; lateral basis bundle) constitutes the remainder of the lateral column, and is continuous in front with the anterior proper fasciculus. It consists chiefly of intersegmental fibers which arise from cells in the gray substance, and, after a longer or shorter course, reënter the gray substance and ramify in it. Some of its fibers are, however, continued upward into the brain under the name of the medial longitudinal fasciculus
Fasciculi in the Posterior Funiculus This funiculus comprises two main fasciculi, viz., the fasciculus gracilis and the fasciculus cuneatus These are separated from each other in the cervical and upper thoracic regions by the postero-intermediate septum, and consist mainly of ascending fibers derived from the posterior nerve roots.
The fasciculus gracilis (tract of Goll) is wedge-shaped on transverse section, and lies next the posterior median septum, its base being at the surface of the medulla spinalis, and its apex directed toward the posterior gray commissure. It increases in size from below upward, and consists of long thin fibers which are derived from the posterior nerve roots, and ascend as far as the medulla oblongata, where they end in the nucleus gracilis.
The fasciculus cuneatus (tract of Burdach) is triangular on transverse section, and lies between the fasciculus gracilis and the posterior column, its base corresponding with the surface of the medulla spinalis. Its fibers, larger than those of the fasciculus gracilis, are mostly derived from the same source, viz., the posterior nerve roots. Some ascend for only a short distance in the tract, and, entering the gray matter, come into close relationship with the cells of the dorsal nucleus; while others can be traced as far as the medulla oblongata, where they end in the gracile and cuneate nuclei.

The fasciculus gracilis and fasciculus cuneatus conduct (1) impulses of conscious muscle sense, neurons of the second order from the nucleus gracilis and nucleus cuneatus, pass in the median lemniscus to the thalamus and neurons of the third order from the thalamus to the cerebral cortex; (2) impulses of unconscious muscle sense, via neurons of the second order from the nucleus gracilis and nucleus cuneatus pass in the internal and external arcuate fibers of the medulla oblongata to the inferior peduncle and through it to the cerebellum; (3) impulses of tactile discrimination, via neurons of the second order from the nucleus cuneatus and nucleus gracilis pass in the median lemniscus to the thalamus, neurons of the third order pass from the thalamus to the cortex.
The Posterior Proper Fasciculus (posterior ground bundle; posterior basis bundle) arises from cells in the posterior column; their axons bifurcate into ascending and descending branches which occupy the ventral part of the funiculus close to the gray column. They are intersegmental and run for varying distances sending off collaterals and terminals to the gray matter.
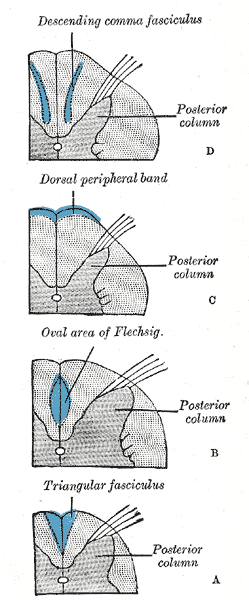
Some descending fibers occupy different parts at different levels. In the cervical and upper thoracic regions they appear as a comma-shaped fasciculus in the lateral part of the fasciculus cuneatus, the blunt end of the comma being directed toward the posterior gray commissure; in the lower thoracic region they form a dorsal peripheral band on the posterior surface of the funiculus; in the lumbar region, they are situated by the side of the posterior median septum, and appear on section as a semi-elliptical bundle, which, together with the corresponding bundle of the opposite side, forms the oval area of Flechsig while in the conus medullaris they assume the form of a triangular strand in the postero-medial part of the fasciculus gracilis. These descending fibers are mainly intersegmental in character and derived from cells in the posterior column, but some consist of the descending branches of the posterior nerve roots. The comma-shaped fasciculus was supposed to belong to the second category, but against this view is the fact that it does not undergo descending degeneration when the posterior nerve roots are destroyed.
Roots of the Spinal Nerves[edit | edit source]
As already stated, each spinal nerve possesses two roots, an anterior and a posterior which are attached to the surface of the medulla spinalis opposite the corresponding column of gray substance (Fig. 675); their fibers become medullated about the fifth month of fetal life.
The Anterior Nerve Root (radix anterior) consists of efferent fibers, which are the axons of the nerve cells in the ventral part of the anterior and lateral columns. A short distance from their origins, these axons are invested by medullary sheaths and, passing forward, emerge in two or three irregular rows over an area which measures about 3 mm. in width.
The Posterior Root (radix posterior) comprises some six or eight fasciculi, attached in linear series along the postero-lateral sulcus. It consists of afferent fibers which arise from the nerve cells in a spinal ganglion. Each ganglion cell gives off a single fiber which divides in a T-shaped manner into two processes, medial and lateral. The lateral processes extend to the sensory end-organs of the skin, muscles, tendons, joints, etc. (somatic receptors), and to the sensory end-organs of the viscera (visceral receptors). The medial processes of the ganglion cells grow into the medulla spinalis as the posterior roots of the spinal nerves.
The posterior nerve root enters the medulla spinalis in three chief bundles, medial, intermediate, and lateral. The medial strand passes directly into the fasciculus cuneatus: it consists of coarse fibers, which acquire their medullary sheaths about the fifth month of intrauterine life; the intermediate strand consists of coarse fibers, which enter the gelatinous substance of Rolando; the lateral is composed of fine fibers, which assume a longitudinal direction in the tract of Lissauer, and do not acquire their medullary sheaths until after birth. In addition to these medullated fibers there are great numbers of non-medullated fibers which enter with the lateral bundle. They are more numerous than the myelinated fibers. They arise from the small cells of the spinal ganglia by T-shaped axons similar to the myelinated. They are distributed with the peripheral nerves chiefly to the skin, only a few are found in the nerves to the muscles. 119 57 Having entered the medulla spinalis, all the fibers of the posterior nerve roots divide into ascending and descending branches, and these in their turn give off collaterals which enter the gray substance (Fig. 676). The descending fibers are short, and soon enter the gray substance. The ascending fibers are grouped into long, short, and intermediate: the long fibers ascend in the fasciculus cuneatus and fasciculus gracilis as far as the medulla oblongata, where they end by arborizing around the cells of the cuneate and gracile nuclei; the short fibers run upward for a distance of only 5 or 6 mm. and enter the gray substance; while the intermediate fibers, after a somewhat longer course, have a similar destination. All fibers entering the gray substance end by arborizing around its nerve cells or the dendrites of cells, those of intermediate length being especially associated with the cells of the dorsal nucleus. 58

The long fibers of the posterior nerve roots pursue an oblique course upward, being situated at first in the lateral part of the fasciculus cuneatus: higher up, they occupy the middle of this fasciculus, having been displaced by the accession of other entering fibers; while still higher, they ascend in the fasciculus gracilis. The upper cervical fibers do not reach this fasciculus, but are entirely confined to the fasciculus cuneatus. The localization of these fibers is very precise: the sacral nerves lie in the medial part of the fasciculus gracilis and near its periphery, the lumbar nerves lateral to them, the thoracic nerves still more laterally; while the cervical nerves are confined to the fasciculus cuneatus (Fig. 673).
Note 113 Lenhossek and Cajal found that in the chick embryo the axons of a few of these nerve cells passed backward through the posterior column, and emerged as the motor fibers of the posterior nerve roots These fibers are said to control the peristaltic movements of the intestine. Their presence, in man, has not yet been determined.
Note 114 Topographical Atlas of the Spinal Cord, 1901.
Note 115 According to Bruce and Pirie (B. M> J., November 17, 1906) this column extends from the middle of the eighth cervical segment to the lower part of the second lumbar or the upper part of the third lumbar segment. Note 116 Somewhat later a change, termed chromatolysis takes place in the nerve cells, and consists of a breaking down and an ultimate disappearance of the Nissl bodies. Further, the body of the cell is swollen, the nucleus displaced toward the periphery, and the part of the axon still attached to the altered cell is diminished in size and somewhat atrophied. Under favorable conditions the cell is capable of reassuming its normal appearance, and its axon may grow again.
Note 117 Schäfer, Proc. Physiolog. Soc., 1899.
Note 118 Ransom, Am. Jour. Anat., 1914; Brain, 1915.
Note 119 Ransom, Brain, 1915, 38.
External links[edit | edit source]
- Spinal Cord Histology – A multitude of great images from the University of Cincinnati
The Nervous System: Sensory and Motor Tracts of the Spinal Cord(link). {{{website}}}. Napa Valley College / Southeast Community College Lincoln, Nebraska.
- eMedicine: Spinal Cord, Topographical and Functional Anatomy
- WebMD. May 17, 2005. Spina Bifida – Topic Overview Information about spina bifida in fetuses and throughout adulthood. WebMD children's health. Retrieved March 19, 2007.
- Potential for spinal injury repair Retrieved February 6, 2008.
- 4000 sets of digital images, showing spatial expression patterns for various genes in adult and juvenile mouse spinal cords from the Allen Institute for Brain Science
- Spinal cord photomicrographs
| Human systems and organs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Nervous system | ||||
|---|---|---|---|---|
|
| Spinal cord | ||||||
|---|---|---|---|---|---|---|
|
Gray's Anatomy[edit source]
- Gray's Anatomy Contents
- Gray's Anatomy Subject Index
- About Classic Gray's Anatomy
- Glossary of anatomy terms
Anatomy atlases (external)[edit source]
[1] - Anatomy Atlases
| This article is a medical stub. You can help WikiMD by expanding it! | |
|---|---|
| Human systems and organs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Anish, Deepika vegiraju, Prab R. Tumpati, MD