Toxocariasis
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Toxocariasis | |
|---|---|

| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Fever, cough, wheezing, abdominal pain, vision loss |
| Complications | Ocular toxocariasis, visceral larva migrans |
| Onset | Variable |
| Duration | Weeks to months |
| Types | N/A |
| Causes | Infection by Toxocara canis or Toxocara cati |
| Risks | Contact with contaminated soil, pet ownership |
| Diagnosis | Serology, ophthalmologic examination |
| Differential diagnosis | Asthma, retinoblastoma, neurocysticercosis |
| Prevention | Deworming pets, avoiding contact with contaminated soil |
| Treatment | Albendazole, mebendazole, corticosteroids |
| Medication | N/A |
| Prognosis | N/A |
| Frequency | Common in areas with high rates of pet ownership |
| Deaths | N/A |
Toxocariasis is human infestation with the larvae of a worm found in the intestines of dogs
Cause[edit | edit source]
Toxocariasis is the parasitic disease caused by the larvae of two species of Toxocara roundworms:
- Toxocara canis from dogs and, less commonly, Toxocara cati from cats.
- Confirmed zoonotic species include the dog roundworm T. canis (presumed most common) and the cat roundworm T. cati (frequency not known). It is not known whether other closely-related Toxocara species can infect humans (e.g. T. malaysiensis of cats).
Neglected tropical disease[edit | edit source]
Toxocariasis is considered one of the Neglected Parasitic Infections.
Transmission[edit | edit source]
- Infected dogs and cats shed Toxocara eggs in their feces into the environment.
- Once in the environment, it takes 2 to 4 weeks for Toxocara larvae to develop inside the eggs and become infectious.
- Toxocara eggs have a strong protective layer, which allows the eggs to survive in the environment for months or even years under the right conditions.
- Humans or other animals (e.g. rabbits, pigs, cattle, or chickens) can be infected by accidentally ingesting Toxocara eggs.
- For example, humans can become infected if they work with dirt and accidentally ingest dirt containing Toxocara eggs.
Undercooked meat[edit | edit source]
Although rare, people can be infected by eating undercooked or raw meat from an infected animal such as a lamb or rabbit. Because dogs and cats are frequently found where people live, there may be large numbers of infected eggs in the environment. Once in the body, the Toxocara eggs hatch and the larvae can travel in the bloodstream to different parts of the body, including the liver, heart, lungs, brain, muscles, or eyes.
Signs and symptoms[edit | edit source]
Most infected people do not have any symptoms. However, in some people, the Toxocara larvae can cause damage to these tissues and organs. The symptoms of toxocariasis, the disease caused by these migrating larvae, include fever, coughing, inflammation of the liver, or eye problems.
Incidence[edit | edit source]
- A U.S. study in 1996 showed that 30% of dogs younger than 6 months deposit Toxocara eggs in their feces; other studies have shown that almost all puppies are born already infected with Toxocara canis.
- Research also suggests that 25% of all cats are infected with Toxocara cati. Infection rates are higher for dogs and cats that are left outside and allowed to eat other animals.
- In humans, it has been found that 5% of the U.S. population has been infected with Toxocara.
- Globally, toxocariasis is found in many countries, and prevalence rates can reach as high as 40% or more in parts of the world.
Risk factors[edit | edit source]
There are several factors that have been associated with higher rates of infection with Toxocara.
- People are more likely to be infected with Toxocara if they own a dog.
- Children and adolescents under the age of 20 are more likely to test positive for Toxocara infection than adults.
- This may be because children are more likely to eat dirt and play in outdoor environments, such as sandboxes, where dog and cat feces can be found. This infection is more common in people living in poverty.
- Geographic location plays a role as well, because Toxocara is more prevalent in hot, humid regions where eggs are able to survive better in the soil.
Life Cycle[edit | edit source]
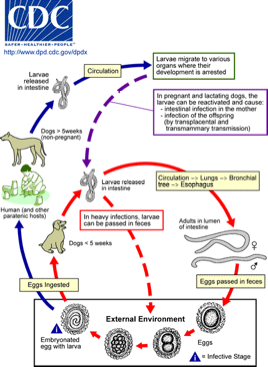
- Toxocara spp. can follow a direct (one host) or indirect (multiple host) life cycle.
- Un-embryonated eggs are shed in the feces of the definitive host (canids: T. canis; felids: T. cati).
- Eggs embryonate over a period of 1 to 4 weeks in the environment and become infective, containing third-stage (L3) larvae.
- Following ingestion by a definitive host, the infective eggs hatch and larvae penetrate the gut wall.
- In younger dogs (T. canis) and in cats (T. cati), the larvae migrate through the lungs, bronchial tree, and esophagus, where they are coughed up swallowed into the gastrointestinal tract; adult worms develop and oviposit in the small intestine.
- In older dogs, patent (egg-producing) infections can also occur, but larvae more commonly become arrested in tissues.
- Arrested larvae are reactivated in female dogs during late gestation and may infect pups by the transplacental (major) and transmammary (minor) routes in whose small intestine adult worms become established.
- In cats, T. cati larvae can be transmitted via the transmammary route to kittens if the dam is infected during gestation, but somatic larval arrest and reactivation does not appear to be important as in T. canis.
Toxocara spp. can also be transmitted indirectly through ingestion of paratenic hosts.
- Eggs ingested by suitable paratenic hosts hatch and larvae penetrate the gut wall and migrate into various tissues where they encyst.
- The life cycle is completed when definitive hosts consume larvae within paratenic host tissue, and the larvae develop into adult worms in the small intestine.
- Humans are accidental hosts who become infected by ingesting infective eggs or undercooked meat/viscera of infected paratenic hosts.
- After ingestion, the eggs hatch and larvae penetrate the intestinal wall and are carried by the circulation to a variety of tissues (liver, heart, lungs, brain, muscle, eyes).
- While the larvae do not undergo any further development in these sites, they can cause local reactions and mechanical damage that causes clinical toxocariasis.
Disease[edit | edit source]
- Most people infected with Toxocara do not have any symptoms.
- There are two major forms of toxocariasis, visceral toxocariasis (VT), also called visceral larva migrans (VLM), and ocular toxocariasis (OT), also called ocular larva migrans (OLM).
- The syndromes VLM and OLM can be caused by infection with the migrating larvae of other kinds of parasites which cause symptoms similar to those caused by migrating Toxocara larvae.
- In a few people who are infected with high numbers of Toxocara larvae or have repeated infections, the larvae can travel through parts of the body such as the liver, lungs, or central nervous system and cause symptoms such as fever, coughing, enlarged liver or pneumonia.
- This form of toxocariasis is called visceral toxocariasis (VT).
- The larvae can also travel to the eye and cause ocular toxocariasis (OT).
- Ocular toxocariasis occurs when a microscopic Toxocara larva enters the eye and causes inflammation and scarring on the retina.
Diagnosis[edit | edit source]
- Diagnosis of either visceral toxocariasis or ocular toxocariasis are based on the presence of signs of VT or OT and history of exposure to a potential source of infectious Toxocara eggs or larvae (e.g. in undercooked infected meat or offal).
- The diagnosis of visceral toxocariasis is based on compatible disease and exposure history with positive results by serological testing.
- The currently recommended test is an enzyme-linked immunosorbent assay (ELISA) with larval stage antigens, usually excretory/secretory antigens are released when infective Toxocara larvae are cultured.
- The specificity of this assay is good although cross reactivity with antibody to the human roundworm, Ascaris lumbricoides, is possible; however, assays employing Toxocara excretory/secretory antigens minimize this problem.
- Positive serological results should be interpreted with consideration of the patient’s clinical status.
- Detectable antibody may be the result of infection in the past.
- Also, seropositivity can be present in asymptomatic Toxocara infection.
- Paired serum samples demonstrating a significant rise in antibody level over time may be useful to confirm active infection.
- In ocular toxocariasis, Toxocara antibody levels in serum can be low or absent despite clinical disease. In some cases, Toxocara antibody can be detected in the aqueous or vitreous fluid samples from the affected eye and may be due to local antibody production or leakage of antibody from the circulation. The ocular fluid sample may be tested at a lower dilution than serum to improve ELISA sensitivity.
Signs and symptoms[edit | edit source]
The manifestations of toxocariasis reflect the number of migrating larvae, where the larvae have migrated in the body, and the degree of immune response and inflammation that developed in response to the presence of the larvae.
- Many infections are asymptomatic.
- In heavy infections, large numbers of larvae may migrate through liver and lungs or other internal organs, causing inflammation and symptomatic disease (VT).
- Signs of VT include fever, cough, wheezing, abdominal pain, and hepatomegaly. Eosinophilia is often present.
- Visceral toxocariasis has been proposed as a cause of asthma; however, there may be multifactorial causes of asthma and further study is needed to establish a causative link between toxocariasis and asthma.
Treatment[edit | edit source]
- Treatment with albendazole or mebendazole is indicated for visceral toxocariasis, although optimal duration of treatment is undefined.
Both drugs are metabolized in the liver; prolonged use of albendazole (weeks to months) has led to development of pancytopenia in some patients with compromised liver function. Patients on long term treatment should be monitored by serial blood cell counts. However, albendazole has been used to treat millions of patients worldwide and in mass drug administration campaigns, and it is considered to be a safe drug with low toxicity record. In addition to antiparasitic therapy, symptomatic therapy including steroid treatment to control inflammation may be indicated.
Drug dose and duration[edit | edit source]
- Albendazole 400 mg by mouth twice a day for five days (both adult and pediatric dosage)
- Mebendazole 100-200 mg by mouth twice a day for five days (both adult and pediatric dosage)
- Oral albendazole is available for human use in the United States.
- Oral mebendazole is available for human use in the United States.
- For ocular toxocariasis, the goal of treatment is to minimize damage to the eye. Systemic antiparasitic treatment with albendazole or mebendazole at the same doses as for visceral disease may be beneficial for active disease. Attempts to surgically remove the larva may be unsuccessful. Control of inflammation in the eye by use of topical or systemic steroids may be indicated. For patients with quiescent disease, improved outcomes may result from surgical intervention to prevent further damage due to chronic inflammation.
- Albendazole
- Mebendazole
Prevention & Control[edit | edit source]
- Controlling Toxocara infection in dogs and cats will reduce the number of infectious eggs in the environment and reduce the risk of infection for people. Have your veterinarian treat your dogs and cats, especially young animals, regularly for worms. This is especially important if your pets spend time outdoors and may become infected again.
There are several things that you can do around your home to make you and your pets safer, including the following:
- Clean your pet’s living area at least once a week; every day is better. Feces should be either buried or bagged and disposed of in the trash. Wash your hands after handling pet waste.
- Do not allow children to play in areas that are soiled with pet or other animal feces and cover sandboxes when not in use to make sure that animals do not get inside and contaminate them.
- Wash your hands with soap and warm water after playing with your pets or other animals, after outdoor activities, and before handling food or eating.
- Teach children the importance of washing hands to prevent infection.
- Teach children that it is dangerous to eat dirt or soil.
- Toxocara eggs have a strong protective layer, which allows the eggs to survive in the environment for months or even years under the right conditions.
- Many common disinfectants are not effective against Toxocara eggs but extreme heat has been shown to kill the eggs.
- Prompt removal of animal feces can help prevent infection since the eggs require 2 to 4 weeks to become infective once they are passed out of the animal.
- Although rare, people can also be infected by eating undercooked or raw meat from an infected animal such as a lamb or rabbit.
- Meat and offal should always be cooked thoroughly and to appropriate temperatures to prevent illness
| Parasitic disease caused by helminthiases | ||||
|---|---|---|---|---|
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD