Paroxysmal nocturnal hemoglobinuria
(Redirected from Paroxysmal nocturnal haemoglobinuria)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Paroxysmal nocturnal hemoglobinuria | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Hemolysis, hemoglobinuria, thrombosis, fatigue |
| Complications | Chronic kidney disease, pulmonary hypertension, aplastic anemia |
| Onset | Usually in adulthood |
| Duration | Chronic |
| Types | N/A |
| Causes | Acquired genetic mutation in PIGA gene |
| Risks | Bone marrow failure, aplastic anemia |
| Diagnosis | Flow cytometry for CD55 and CD59 |
| Differential diagnosis | Autoimmune hemolytic anemia, myelodysplastic syndrome |
| Prevention | N/A |
| Treatment | Eculizumab, ravulizumab, anticoagulation |
| Medication | N/A |
| Prognosis | Variable; improved with treatment |
| Frequency | 1-2 per million per year |
| Deaths | N/A |
Paroxysmal nocturnal hemoglobinuria[edit | edit source]
Other Names: PNH; Marchiafava-Micheli disease Paroxysmal nocturnal hemoglobinuria is an acquired disorder that leads to the premature death and impaired production of blood cells. The disorder affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal). Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage).
Cause[edit | edit source]
Mutations in the PIGA gene cause paroxysmal nocturnal hemoglobinuria. The PIGA gene provides instructions for making a protein called phosphatidylinositol glycan class A. This protein takes part in a series of steps that produce a molecule called GPI anchor. GPI anchor attaches many different proteins to the cell membrane, thereby ensuring that these proteins are available when needed at the surface of the cell. Some gene mutations are acquired during a person's lifetime and are present only in certain cells. These changes, which are called somatic mutations, are not inherited. In people with paroxysmal nocturnal hemoglobinuria, somatic mutations of the PIGA gene occur in blood-forming cells called hematopoietic stem cells, which are found mainly in the bone marrow. These mutations result in the production of abnormal blood cells. As the abnormal hematopoietic stem cells multiply, increasing numbers of abnormal blood cells are formed, alongside normal blood cells produced by normal hematopoietic stem cells. The premature destruction of red blood cells seen in paroxysmal nocturnal hemoglobinuria is caused by a component of the immune system called complement. Complement consists of a group of proteins that work together to destroy foreign invaders such as bacteria and viruses. To protect the individual's own cells from being destroyed, this process is tightly controlled by complement-regulating proteins. Complement-regulating proteins normally protect red blood cells from destruction by complement. In people with paroxysmal nocturnal hemoglobinuria, however, abnormal red blood cells are missing two important complement-regulating proteins that need the GPI anchor protein to attach them to the cell membrane. These red blood cells are prematurely destroyed, leading to hemolytic anemia. Research suggests that certain abnormal white blood cells that are also part of the immune system may mistakenly attack normal blood-forming cells, in a malfunction called an autoimmune process. In addition, abnormal hematopoietic stem cells in people with paroxysmal nocturnal hemoglobinuria may be less susceptible than normal cells to a process called apoptosis, which causes cells to self-destruct when they are damaged or unneeded. These features of the disorder may increase the proportion of abnormal blood cells in the body. The proportion of abnormal blood cells affects the severity of the signs and symptoms of paroxysmal nocturnal hemoglobinuria, including the risk of hemoglobinuria and thrombosis.
Inheritance[edit | edit source]
This condition is acquired, rather than inherited. It results from new mutations in the PIGA gene, and generally occurs in people with no previous history of the disorder in their family. The condition is not passed down to children of affected individuals.
Symptoms[edit | edit source]
Symptoms may include:
- Abdominal pain
- Back pain
- Blood clots, may form in some people
- Dark urine, comes and goes
- Easy bruising or bleeding
- Headache
- Shortness of breath
- Weakness, fatigue
- Pallor
- Chest pain
- Difficulty swallowing
For most diseases, symptoms will vary from person to person. People with the same disease may not have all the symptoms listed. 80%-99% of people have these symptoms
- Fatigue(Tired)
- Hemolytic anemia
30%-79% of people have these symptoms
- Bone marrow hypocellularity(Bone marrow failure)
- Hypercoagulability
- Thromboembolism
5%-29% of people have these symptoms
- Abdominal pain(Pain in stomach)
- Abnormal bleeding(Bleeding tendency)
- Abnormal renal physiology(Abnormal kidney function)
- Angina pectoris
- Aplastic anemia
- Cerebral artery stenosis(Narrowing of a cerebral artery)
- Dysphagia(Poor swallowing)
- Hemoglobinuria(Hemoglobin in urine)
- Hypoplastic anemia
- Muscle weakness(Muscular weakness)
- Myelodysplasia
- Myocardial infarction(Heart attack)
- Pallor
- Pulmonary arterial hypertension(Increased blood pressure in blood vessels of lungs)
- Pulmonary embolism(Blood clot in artery of lung)
- Transient ischemic attack(Mini stroke)
Diagnosis[edit | edit source]
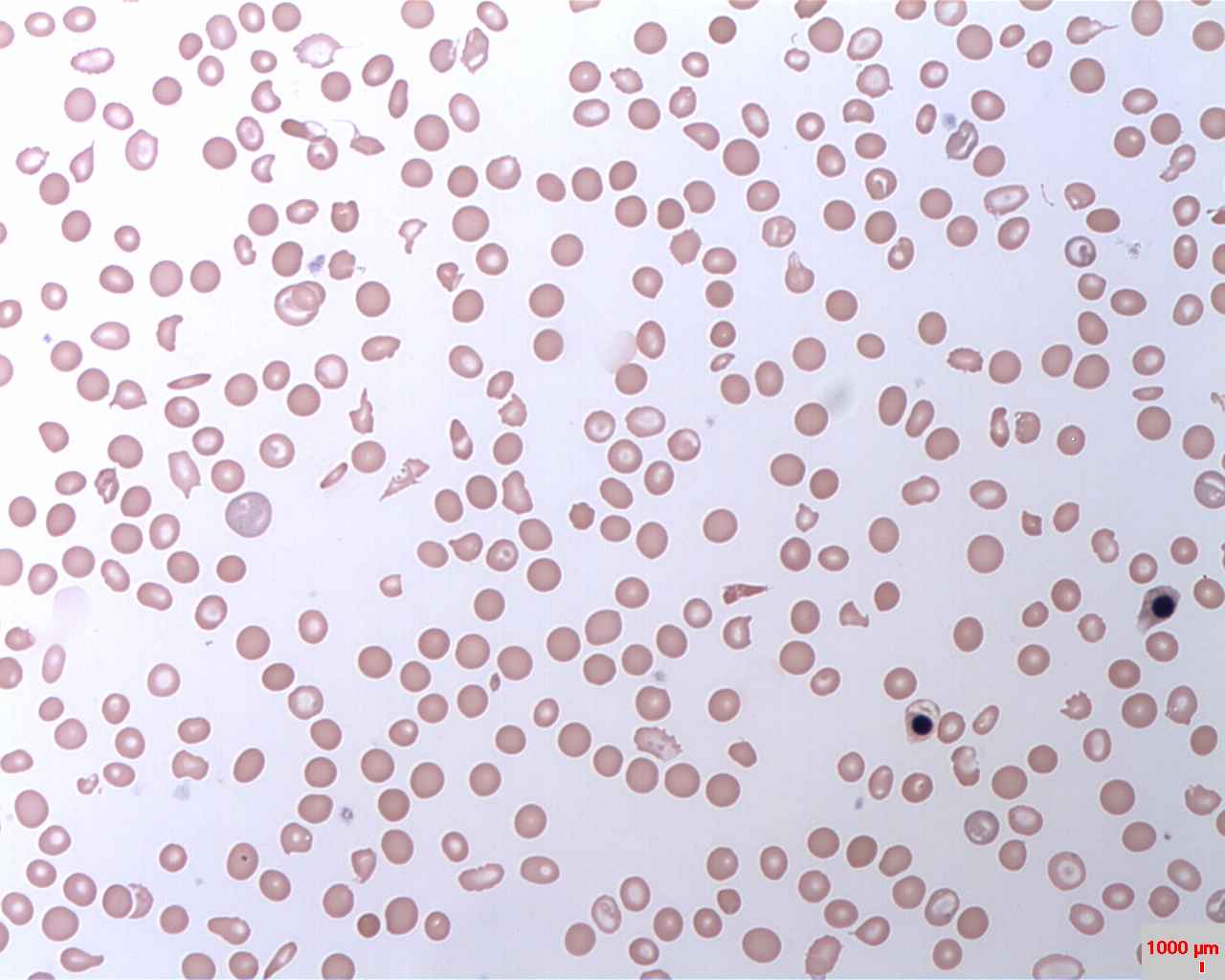
Red and white blood cell counts and platelet counts may be low. Red or brown urine signals the breakdown of red blood cells and that hemoglobin is being released into the body's circulation and eventually into the urine. Tests that may be done to diagnose this condition include:
- Complete blood count (CBC)
- Coombs test
- Flow cytometry to measure certain proteins
- Ham (acid hemolysin) test
- Serum hemoglobin and haptoglobin
- Sucrose hemolysis test
- Urinalysis
- Urine hemosiderin, urobilinogen, hemoglobin
- LDH test
- Reticulocyte count
Treatment[edit | edit source]
Steroids or other medicines that suppress the immune system may help slow the breakdown of red blood cells. Blood transfusions may be needed. Supplemental iron and folic acid are provided. Blood thinners may also be needed to prevent clots from forming. Soliris (eculizumab) is a drug used to treat PNH. It blocks the breakdown of red blood cells. Bone marrow transplantation can cure this disease. It may also stop the risk of developing PNH in people with aplastic anemia. All people with PNH should receive vaccinations against certain types of bacteria to prevent infection. Ask your health care provider which ones are right for you. The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition.
- Eculizumab(Brand name: Soliris)eculizumab (Soliris) was approved for the treatment of paroxysmal nocturnal hemoglobinuria to reduce hemolysis.
- Ravulizumab-cwvz (Brand name: Ultomiris) ravulizumab-cwvz (Ultomiris) was approved for the treatment of adult patients with paroxysmal nocturnal hemoglobinuria (PNH).
Prognosis[edit | edit source]
The outcome varies. Most people survive for more than 10 years after their diagnosis. Death can result from complications such as blood clot formation (thrombosis) or bleeding. In rare cases, the abnormal cells may decrease over time.
| Diseases of red blood cells | ||||
|---|---|---|---|---|
|
| Immune disorders: Lymphoid and complement immunodeficiency (D80–D85, 279.0–4) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Inborn error of lipid metabolism: Phospholipid metabolism disorders | ||||
|---|---|---|---|---|
|
NIH genetic and rare disease info[edit source]
Paroxysmal nocturnal hemoglobinuria is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Paroxysmal nocturnal hemoglobinuria
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Kondreddy Naveen, Prab R. Tumpati, MD


