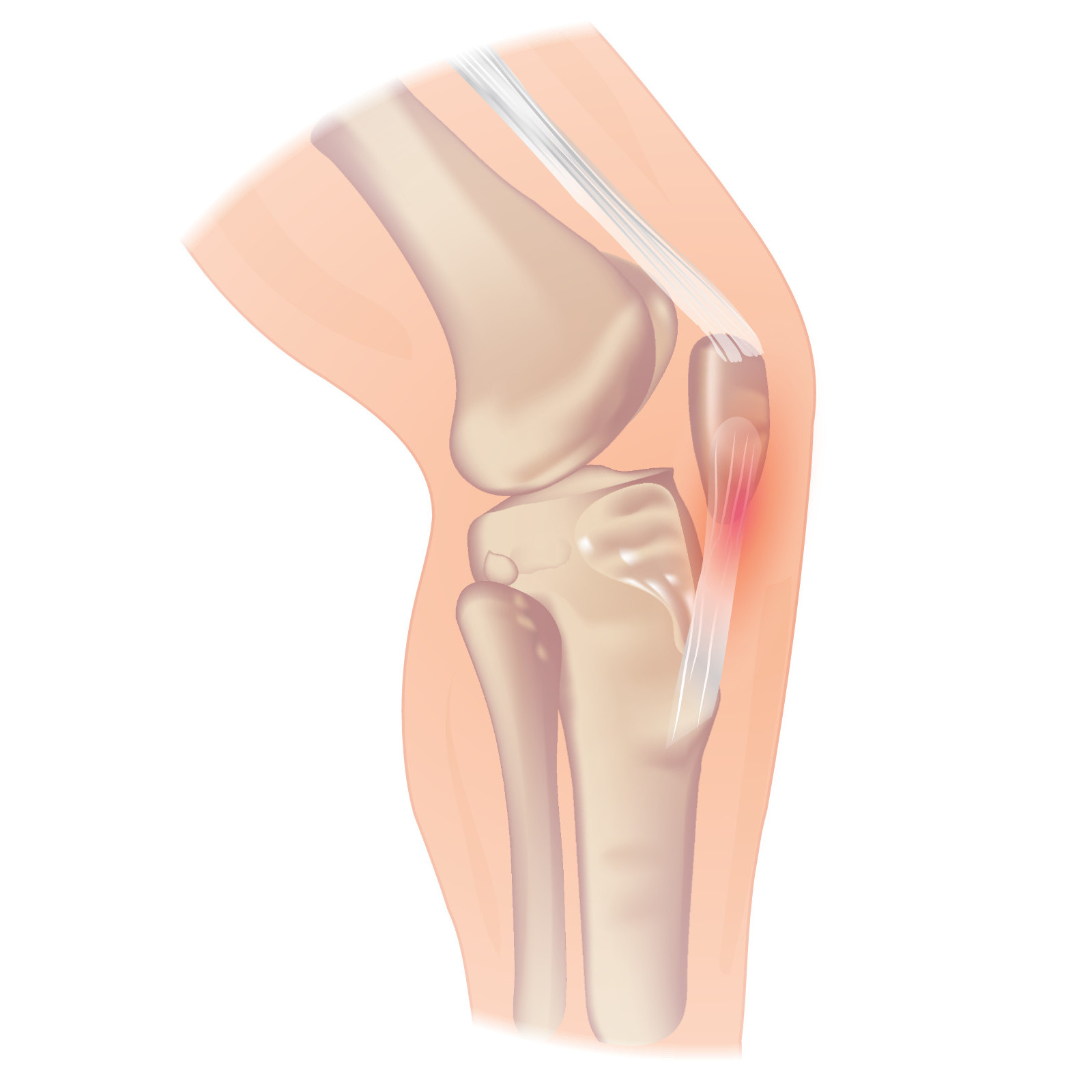
Patellar tendinitis
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Patellar tendinitis | |
|---|---|
| |
| Synonyms | Jumper's knee |
| Pronounce | N/A |
| Specialty | Sports medicine, Orthopedics |
| Symptoms | Knee pain, swelling |
| Complications | N/A |
| Onset | Gradual |
| Duration | Weeks to months |
| Types | N/A |
| Causes | Overuse, repetitive stress |
| Risks | Athletics, jumping sports |
| Diagnosis | Physical examination, imaging |
| Differential diagnosis | Patellofemoral pain syndrome, Osgood-Schlatter disease |
| Prevention | N/A |
| Treatment | Rest, physical therapy, NSAIDs |
| Medication | N/A |
| Prognosis | Good with treatment |
| Frequency | Common in athletes |
| Deaths | N/A |
Alternate names[edit | edit source]
- Patellar tendinopathy
- Jumper's knee
Definition[edit | edit source]
- “Jumper's knee,” also called patellar tendinopathy, is a painful condition of the knee, mainly activity-related, caused by small tears in the patellar tendon that mainly occurs in sports requiring strenuous jumping and results in a localized patellar tendon tenderness. The tears are typically caused by accumulated stress on the patellar or quadriceps tendon.
Etiology[edit | edit source]
- Jumper's knee is an overuse injury of the knee extensor mechanism due to repetitive mechanical stress from athletic activities requiring movements such as jumping, landing, acceleration, deceleration, and cutting.
- Micro-tearing of the knee extensor tendons can arise after constant repetition of these movements during a single exercise session or if there is insufficient rest between sessions.
- There are several intrinsic factors of the knee that predispose to this pathology. These include ligamentous laxity, quadriceps and hamstring tightness, excessive Q-angle of the knee, abnormal patellar height, previous ongoing inflammation of the knee, and excessive force generation on the knee.
- Other possible risk factors are the weight, body mass index, waist-to-hip ratio, leg-length difference, the arch height of the foot, quadriceps strength, and vertical jump performance. These factors can result in increased strain on the patellar tendon.
Epidemiology[edit | edit source]
- Since sports injuries often are under-reported, it is hard to determine the exact frequency of patellar tendinopathy both in the United States and on an international scale. Jumping sports such as volleyball, basketball, and long and high jumps have a high prevalence of the disease.
- Jumper's knee occurs more often in males.
Staging[edit | edit source]
Blazina et al. first used the term jumper's knee in 1973. They also classified the pathology by stage according to the onset of pain in relation to physical activity. This classification along with its modifications is still widely employed. Blazina et al. suggest 4 stages.
- Stage 1: Pain after sports activity
- Stage 2: Pain at the beginning of sports activity yet disappearing with warm-up and sometimes reappearing with fatigue
- Stage 3: Pain at rest and during activity along with the deterioration of performance.
- Stage 4: Rupture of the tendon
It may be useful to classify the pathology into 3 stages according to the duration of symptoms.
- Acute when symptoms have been present for 0 to 6 weeks
- Sub-acute when symptoms have been present between 6 to 12 weeks
- Chronic after more than 3 months
Signs and symptoms[edit | edit source]
- The patient will usually complain of well-localized pain and tenderness on the inferior tip of the patella.
- Pain with prolonged sitting, squatting, and stair climbing.
- Patients may complain of pain from activities that involve prolonged Flexion of the knee, otherwise known as the " Movie Theater sign".
- Sudden tendon pain occurs with loading and usually stops almost immediately when the load is removed. Rarely a patient feels pain when they are resting.
- Basset's sign "passive extension – flexion sign" where the examiner palpates the anterior aspect of the fully extended knee and identifies the highest tender point which is usually at the inferior pole of the patella and the proximal part of the patellar tendon. The examination is repeated in 90 degrees of knee flexion and the sign is positive when there is a marked reduction in tenderness to palpation in the flexed knee position.
- The other sign is the "standing active quadriceps sign" where the whole patellar tendon is palpated whilst the patient is standing and the examination is repeated whilst the patient is standing on the involved extremity with the knee in 30 degrees of flexion. Similarly, the sign is positive if there is a marked reduction in tenderness to palpation whilst the quadriceps muscle is contracted.
Diagnosis[edit | edit source]
- Currently, there is no widely accepted gold standard diagnostic technique. Ultrasound offers several advantages; it is time and cost-saving, it is non-invasive, repeatable, and accurate, and provides a dynamic image of the knee structures.
- Radiograph including anteroposterior, lateral, and skyline views are recommended to exclude any acute bony injuries or pathologies. Radiographic changes on the tendon might be noted such as elongation of the involved pole of the patella, calcification, inferior traction spur known as enthesophyte in chronic cases, and increased density within the patellar tendon matrix. However, these changes are rare in the first six months of symptoms.
- MRI (Magnetic resonance imaging) would be indicated in chronic cases and for surgical planning. It can show thickening of the patellar tendon which is more diagnostic than the presence of edema.
Management[edit | edit source]
Most patients with jumper's knee are managed through medical and rehabilitative treatment in the initial stages of the disease.
- Non-surgical treatment focusing on the following: Relative rest rather than immobilization to avoid tendon and muscle atrophy. Cryotherapy provides analgesia and antagonizes the Neovascularization process which contributes to the pathology. Modification of activities, and sports training including adequate warm-ups, and physiotherapy to increase the flexibility of quadriceps and hamstring muscles. Eccentric training has been suggested to play a key role in the rehabilitation of a jumper's knee. Eccentric training has been shown to have equally efficacious results to that of surgical treatment. It is recommended that eccentric training should be tried for twelve weeks before offering surgical treatment.
- Surgical treatment is usually indicated in cases of partial tendon tears and Blazina stage III where pain continues during rest and activities. Also, it remains the last resort for chronic refractory cases unresponsive to conservative treatment. Traditionally, the gold standard for surgical treatment of patellar tendinopathy involved open debridement of the inferior pole of the patella, as well as debridement of the patellar tendon by excising the angiofibroblastic and degenerative areas. This is followed by reattachment of the tendon using sutures or anchors as indicated. Recently, knee Arthroscopy has gained popularity for tissue debridement and release. The arthroscopic procedure has been described to be performed through a direct inferior patellar portal.
Differential diagnosis[edit | edit source]
- Osgood-Schlatter disease
- meniscal injuries
- quadriceps injury
- patellofemoral syndrome
- knee bursitis
- osteochondritis dissecans
- patellar Subluxation
Prognosis[edit | edit source]
- Most cases of patellar tendinopathy will resolve with nonoperative management.[10] Nevertheless, mild to moderate pain may persist for 15 years in adult athletes with patellar tendinopathy but does not appear to limit leisure-time physical activity.
Complications[edit | edit source]
- There are multiple pitfalls to be aware of, including the failure to control pain. The athlete’s beliefs about pain and pathology may influence the development and management of unresponsive tendinopathies. Because some athletes may have been told that they have weakened tendons due to tears and degeneration, and hence an increased risk of rupture, they may develop fear-avoidance behavior, which can be associated with poorer functional outcomes in individuals suffering from lower-limb tendinopathy. Over-reliance on non-invasive therapies like shockwave therapy and injections instead of including rehabilitation exercises as part of the treatment plan can also lead to complications.
References[edit | edit source]
- Javier A. Santana; Ahmed Mabrouk; Andrew l. Sherman. Jumper's knee.[Updated March 17, 2021]. In StatPearls (Internet). Available at: https://www.ncbi.nlm.nih.gov/books/NBK532969/
- U Fredberg, L Bolvig. Jumper's knee. Review of the literature April 1999. Available at: https://pubmed.ncbi.nlm.nih.gov/10220839/
| Soft tissue disorders | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD


