Bronchiolitis obliterans
(Redirected from Obliterative bronchiolitis)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Bronchiolitis obliterans | |
|---|---|
| |
| Synonyms | Obliterative bronchiolitis, constrictive bronchiolitis |
| Pronounce | N/A |
| Specialty | Pulmonology |
| Symptoms | Cough, shortness of breath, wheezing |
| Complications | Respiratory failure, pulmonary hypertension |
| Onset | Gradual |
| Duration | Long-term |
| Types | N/A |
| Causes | Inhalation injury, lung transplant rejection, rheumatoid arthritis, viral infection |
| Risks | Smoking, exposure to toxic fumes |
| Diagnosis | Pulmonary function test, CT scan, lung biopsy |
| Differential diagnosis | Asthma, chronic obstructive pulmonary disease |
| Prevention | N/A |
| Treatment | Corticosteroids, immunosuppressive drugs, lung transplant |
| Medication | N/A |
| Prognosis | Variable, often poor |
| Frequency | Rare |
| Deaths | N/A |
Obliterative bronchiolitis[edit | edit source]
Bronchiolitis obliterans is an inflammatory condition that affects the lung's tiniest airways, the bronchioles. In affected people, the bronchioles may become damaged and inflamed leading to extensive scarring that blocks the airways.
Epidemiology[edit | edit source]
Bronchiolitis obliterans syndrome is considered as a form of chronic allograft rejection after lung transplantation. The majority of lung transplant recipients who are long term survivors develop bronchiolitis obliterans syndrome. More than 50% of recipients will develop some degree of BO by 5 years post-transplant. The average time to diagnose BO is 16 to 20 months after lung transplant but has been reported as early as 3 months after transplantation. About 5% to 14% of Hematopoietic stem cell transplantation (HSCT) recipients also develop bronchiolitis obliterans syndrome which is pulmonary graft vs. host disease and can present several months to years later after transplantation.
Cause[edit | edit source]
Bronchiolitis obliterans may result from lung injury caused by a variety of different chemicals and respiratory infections. Inhaled chemicals known to irritate the lungs and lead to the condition include chlorine; ammonia; oxides of nitrogen or sulfur dioxide; welding fumes; or food flavoring fumes (such as diacetyl). Respiratory infections caused by respiratory syncytial virus, adenovirus, or Mycoplasma pneumonia have been linked with the condition.
Bronchiolitis obliterans can also be associated with rheumatoid arthritis and graft-versus-host disease following a lung or hematopoietic cell transplantation.
Inheritance[edit | edit source]
Bronchiolitis obliterans is not thought to be inherited. Most cases occur sporadically in people with no family history of the condition.
Signs and symptoms[edit | edit source]
Signs and symptoms of bronchiolitis obliterans generally develop approximately two to eight weeks after exposure to toxic fumes or a respiratory illness. Affected people may experience a dry cough, shortness of breath, and/or wheezing. Fatigue and wheezing in the absence of a cold or asthma may also be noted. Symptoms generally progress slowly over weeks to months. A physical exam may reveal decreased breath sounds and prolonged expiratory phase with or without wheeze usually both in inspiratory and expiratory phase. Rales may also be noted in some cases. Cases of bronchiolitis obliterans associated with Castleman’s disease may also have paraneoplastic pemphigus which may present with oral ulcers as well as lymphadenopathy.
Diagnosis[edit | edit source]
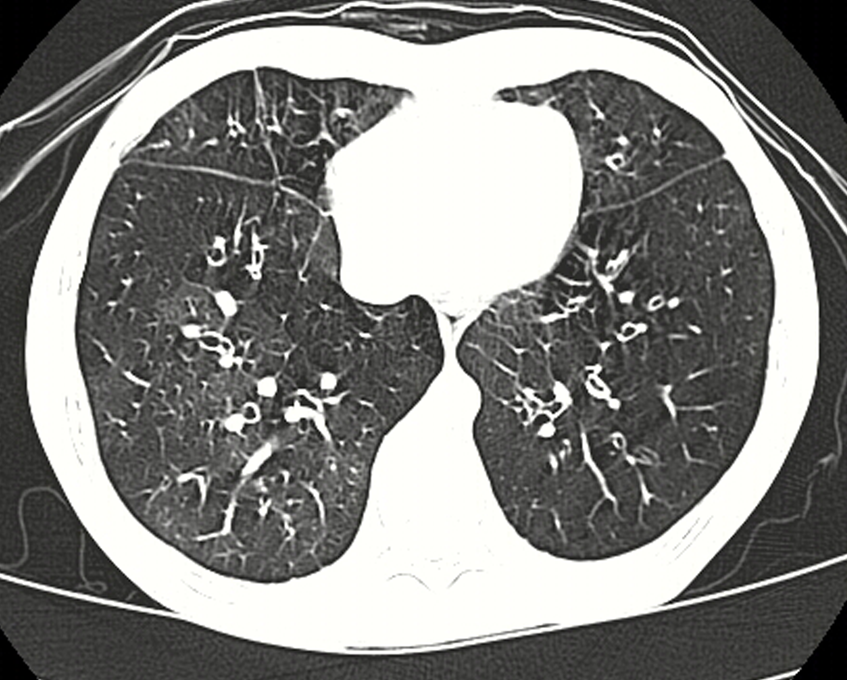
A diagnosis of bronchiolitis obliterans is often suspected based on the presence of characteristic signs and symptoms. Additional testing can then be ordered to support and confirm the diagnosis. These tests may include:
- Imaging studies (such as a chest CT scan)
- Pulmonary function tests
- Surgical lung biopsy (gold standard)
Treatment[edit | edit source]
Although there is no cure for bronchiolitis obliterans, treatment may help stabilize or slow its progression. The best treatment options and the effectiveness of the selected treatments vary based on the underlying cause and the severity of the condition. Medications often prescribed to people with bronchiolitis obliterans include certain types of antibiotics (called macrolide antibiotics), corticosteroids, and immunosuppressive drugs. In severe cases, lung transplantation may be recommended. Therapies such as cough suppressors or supplemental oxygen can also be given to manage the symptoms associated with the condition.
| Diseases of the respiratory system | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info[edit source]
Bronchiolitis obliterans is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Bronchiolitis obliterans
|
Transform your life with W8MD's budget GLP1 injections from $125
W8MD offers a medical weight loss program NYC and a clinic to lose weight in Philadelphia. Our W8MD's physician supervised medical weight loss centers in NYC provides expert medical guidance, and offers telemedicine options for convenience.
Why choose W8MD?
- Comprehensive care with FDA-approved weight loss medications including:
- loss injections in NYC both generic and brand names:
- weight loss medications including Phentermine, Qsymia, Diethylpropion etc.
- Accept most insurances for visits or discounted self pay cost.
- Generic weight loss injections starting from just $125.00 for the starting dose
- In person weight loss NYC and telemedicine medical weight loss options in New York city available
- Budget GLP1 weight loss injections in NYC starting from $125.00 biweekly with insurance!
Book Your Appointment
Start your NYC weight loss journey today at our NYC medical weight loss, and Philadelphia medical weight loss Call (718)946-5500 for NY and 215 676 2334 for PA
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD






