Mucormycosis
(Redirected from Rhinocerebral mucormycosis)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Mucormycosis | |
|---|---|
| |
| Synonyms | Zygomycosis, phycomycosis |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Fever, headache, cough, nasal congestion, facial swelling, black lesions on the nasal bridge or upper inside of the mouth |
| Complications | Tissue necrosis, blindness, cerebral infarction, death |
| Onset | Rapid |
| Duration | Variable |
| Types | N/A |
| Causes | Fungi of the order Mucorales |
| Risks | Diabetes mellitus, neutropenia, organ transplantation, iron overload, immunosuppression |
| Diagnosis | Biopsy, culture, imaging studies |
| Differential diagnosis | Aspergillosis, bacterial sinusitis, Wegener's granulomatosis |
| Prevention | N/A |
| Treatment | Antifungal medication (e.g., amphotericin B), surgical debridement |
| Medication | N/A |
| Prognosis | Poor if untreated |
| Frequency | Rare |
| Deaths | N/A |
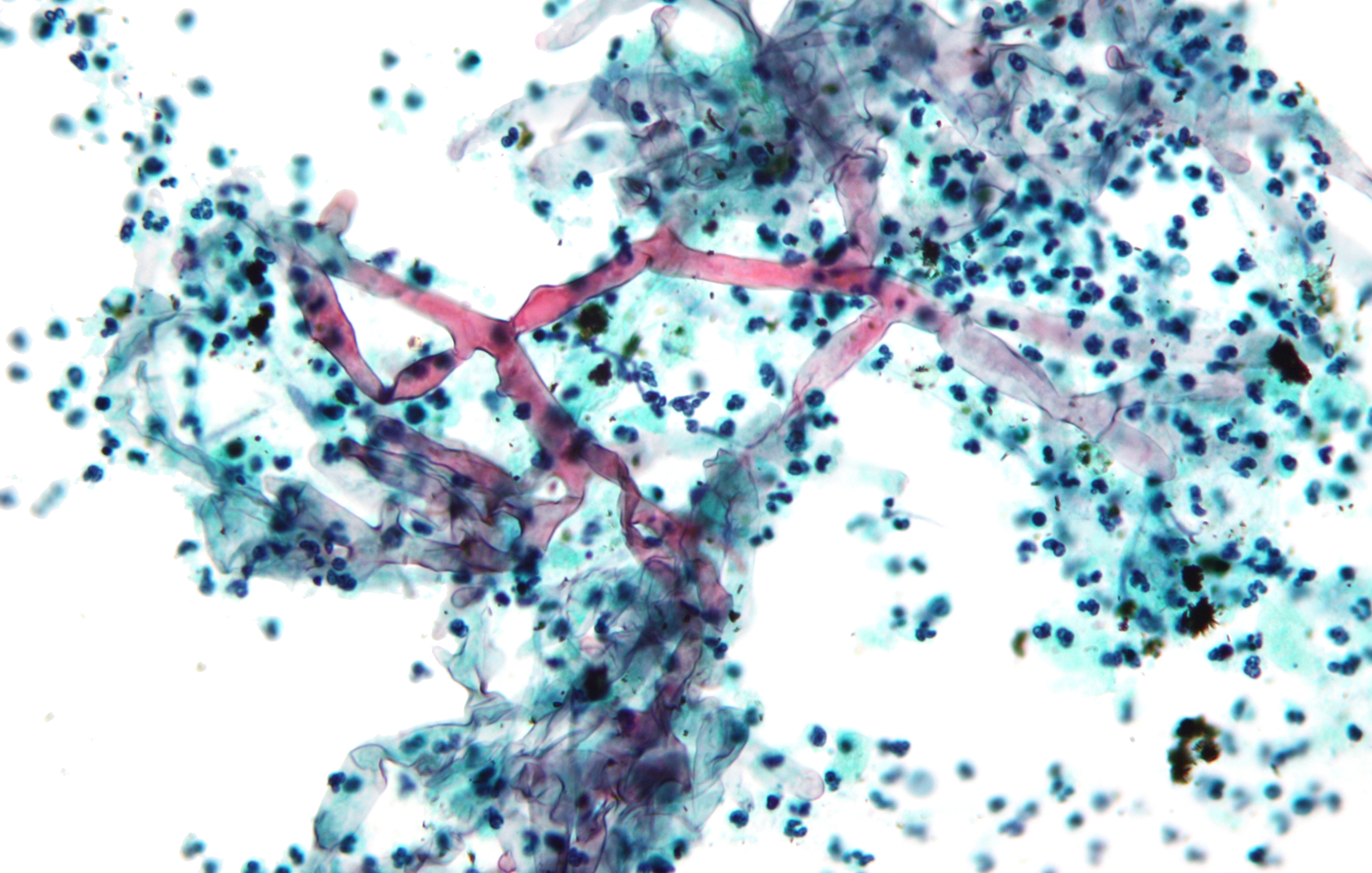
Mucormycosis is any fungal infection caused by fungi in the order Mucorales.
Mucormycosis (previously called zygomycosis) is a serious but rare fungal infection caused by a group of molds called mucormycetes. These molds live throughout the environment. Mucormycosis mainly affects people who have health problems or take medicines that lower the body’s ability to fight germs and sickness. It most commonly affects the sinuses or the lungs after inhaling fungal spores from the air, or the skin after the fungus enters the skin through a cut, burn, or other type of skin injury.
Etiologic agent[edit | edit source]
Molds belonging to the order Mucorales, most commonly Rhizopus species. Others include Mucor species, Cunninghamella bertholletiae, Apophysomyces species, and Lichtheimia (formerly Absidia) species.
Reservoir[edit | edit source]
Mucormycetes are thermotolerant molds that are found in the environment. Environmental sampling studies indicate that Mucormycetes are commonly found in soil, but are rarely found in air samples targeting fungal spores. Specific environmental niches vary among genera and species.
Transmission[edit | edit source]
Transmission occurs through inhalation, inoculation, or ingestion of spores from the environment. Although most cases are sporadic, healthcare-associated outbreaks have been linked to adhesive bandages, wooden tongue depressors, hospital linens, negative pressure rooms, water leaks, poor air filtration, non-sterile medical devices, and building construction. Community-onset outbreaks have been associated with trauma sustained during natural disasters.
Types of mucormycosis[edit | edit source]
Rhinocerebral (sinus and brain) mucormycosis is an infection in the sinuses that can spread to the brain. This form of mucormycosis is most common in people with uncontrolled diabetes and in people who have had a kidney transplant. Pulmonary (lung) mucormycosis is the most common type of mucormycosis in people with cancer and in people who have had an organ transplant or a stem cell transplant. Gastrointestinal mucormycosis is more common among young children than adults, especially premature and low birth weight infants less than 1 month of age, who have had antibiotics, surgery, or medications that lower the body’s ability to fight germs and sickness. Cutaneous (skin) mucormycosis: occurs after the fungi enter the body through a break in the skin (for example, after surgery, a burn, or other type of skin trauma). This is the most common form of mucormycosis among people who do not have weakened immune systems. Disseminated mucormycosis occurs when the infection spreads through the bloodstream to affect another part of the body. The infection most commonly affects the brain, but also can affect other organs such as the spleen, heart, and skin.Symptoms of Mucormycosis
The symptoms of mucormycosis depend on where in the body the fungus is growing. 1,4 Contact your healthcare provider if you have symptoms that you think are related to mucormycosis. Symptoms of rhinocerebral (sinus and brain) mucormycosis include:
- One-sided facial swelling
- Headache
- Nasal or sinus congestion
- Black lesions on nasal bridge or upper inside of mouth that quickly become more severe
- Fever
Symptoms of pulmonary (lung) mucormycosis include:
- Fever
- Cough
- Chest pain
- Shortness of breath
- Cutaneous (skin) mucormycosis can look like blisters or ulcers, and the infected area may turn black. Other symptoms include pain, warmth, excessive redness, or swelling around a wound.
Symptoms of gastrointestinal mucormycosis include:
- Abdominal pain
- Nausea and vomiting
- Gastrointestinal bleeding
Disseminated mucormycosis typically occurs in people who are already sick from other medical conditions, so it can be difficult to know which symptoms are related to mucormycosis. Patients with disseminated infection in the brain can develop mental status changes or coma.
Risk factors[edit | edit source]
Mucormycosis is rare, but it’s more common among people who have health problems or take medicines that lower the body’s ability to fight germs and sickness. Certain groups of people are more likely to get mucormycosis, including people with:
- Diabetes, especially with diabetic ketoacidosis
- Cancer
- Organ transplant
- Stem cell transplant
- Neutropenia
- Long-term corticosteroid use
- Injection drug use
- Too much iron in the body (iron overload or hemochromatosis)
- Skin injury due to surgery, burns, or wounds
- Prematurity and low birthweight (for neonatal gastrointestinal mucormycosis)
Diagnosis[edit | edit source]
- A definitive diagnosis of mucormycosis typically requires histopathological evidence or positive culture from a specimen from the site of infection.
- Specimens from sterile body sites offer stronger evidence of invasive infection compared to colonization.
- Culture of non-sterile sites (e.g., sputum) may be helpful in patients with infection that is clinically consistent with mucormycosis. Mucormycetes may be difficult to differentiate from other filamentous fungi in tissue; experienced pathological and microbiological assistance is often helpful.
- No routine serologic tests for mucormycosis are currently available, and blood tests such as beta-D-glucan or Aspergillus galactomannan do not detect mucormycetes.
- DNA-based techniques for detection are promising but are not yet fully standardized or commercially available
Treatment[edit | edit source]
- Mucormycosis is a serious infection and needs to be treated with prescription antifungal medicine, usually amphotericin B, posaconazole, or isavuconazole.
- These medicines are given through a vein (amphotericin B, posaconazole, isavuconazole) or by mouth (posaconazole, isavuconazole).
- Other medicines, including fluconazole, voriconazole, and echinocandins, do not work against fungi that cause mucormycosis.
- Often, mucormycosis requires surgery to cut away the infected tissue.
Sequelae[edit | edit source]
The overall prognosis depends on several factors, including the rapidity of diagnosis and treatment, the site of infection, and the patient’s underlying conditions and degree of immunosuppression.
Mortality[edit | edit source]
The overall mortality rate is approximately 50%, although early identification and treatment can lead to better outcomes.
Gallery[edit | edit source]
Map of COVID-associated Mucormycosis
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD






