Sporotrichosis
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Sporotrichosis | |
|---|---|
| Synonyms | Rose gardener's disease |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Skin lesions, ulcers, lymph node swelling |
| Complications | Disseminated infection |
| Onset | 1 to 12 weeks after exposure |
| Duration | Weeks to months |
| Types | N/A |
| Causes | Sporothrix schenckii complex |
| Risks | Handling soil, plants, sphagnum moss |
| Diagnosis | Culture, biopsy |
| Differential diagnosis | Cutaneous leishmaniasis, mycobacterial infection |
| Prevention | Protective clothing, avoiding exposure |
| Treatment | Itraconazole, amphotericin B |
| Medication | Antifungals |
| Prognosis | Generally good with treatment |
| Frequency | Common in tropical and subtropical areas |
| Deaths | N/A |
Sporotrichosis is an infection with a fungus acquired through a skin wound; causes an ulcer at the site of infection and small, rounded masses of tissue near it.
Pathophysiology[edit | edit source]
Sporotrichosis (also known as “rose gardener’s disease”) is an infection caused by a fungus called Sporothrix.
Habitat[edit | edit source]
This fungus lives throughout the world in soil and on plant matter such as sphagnum moss, rose bushes, and hay.
Source of infection[edit | edit source]
People get sporotrichosis by coming in contact with the fungal spores in the environment. Cutaneous (skin) infection is the most common form of the infection. It occurs when the fungus enters the skin through a small cut or scrape, usually after someone touches contaminated plant matter. Skin on the hands or arms is most commonly affected.
Types of sporotrichosis[edit | edit source]
Cutaneous (skin) sporotrichosis is the most common form of the infection. It usually occurs on a person’s hand or the arm after touching contaminated plant matter. Pulmonary (lung) sporotrichosis is rare but can happen after someone breathes in fungal spores from the environment. Disseminated sporotrichosis occurs when the infection spreads to another part of the body, such as bones, joints, or central nervous system. This form of sporotrichosis usually affects people with health problems or who take medicines that lower the body’s ability to fight germs and sickness, such as people living with HIV.
Other forms: Sporothrix brasiliensis[edit | edit source]
Sporothrix brasiliensis is a fungus that is increasingly causing disease in cats and people in Brazil and parts of South America.
Symptoms[edit | edit source]
The symptoms of sporotrichosis depend on where the fungus is growing in the body. Contact your healthcare provider if you have symptoms that you think are related to sporotrichosis. Sporotrichosis usually affects the skin or tissues underneath the skin. The first symptom of cutaneous (skin) sporotrichosis is usually a small, painless bump that can develop any time from 1 to 12 weeks after exposure to the fungus. The bump can be red, pink, or purple, and usually appears on the finger, hand, or arm where the fungus has entered through a break in the skin. The bump will eventually grow larger and may look like an open sore or ulcer that is very slow to heal. Additional bumps or sores may appear later near the original one. Pulmonary (lung) sporotrichosis is rare. Symptoms include cough, shortness of breath, chest pain, and fever. Symptoms of disseminated sporotrichosis depend on the body part affected. For example, infection of the joints can cause joint pain that may be confused with rheumatoid arthritis. Infections of the central nervous system can involve difficulty thinking, headache, and seizures.
Risk & Prevention[edit | edit source]
People who touch plant matter such as sphagnum moss, rose bushes, or hay are more likely to become infected. For example, sporotrichosis outbreaks have occurred among forestry workers, people who work in tree nurseries and garden centers, and people who handle hay bales. The severe forms of sporotrichosis (those that affect the lungs, bones or joints, or central nervous system) usually affect people with weakened immune systems or other diseases including diabetes, chronic obstructive pulmonary disease (COPD), alcoholism, or HIV.
Reduce risk[edit | edit source]
You can lower the chance of getting sporotrichosis by wearing protective clothing such as gloves and long sleeves when touching plant matter that can cause minor cuts or scrapes.
In Brazil, people have gotten sporotrichosis from contact with cats. This form of sporotrichosis (Sporothrix brasiliensis) has not been found in the United States. Be careful with unfamiliar animals, particularly cats. Cat bites and scratches can spread the fungus that causes sporotrichosis, and other diseases. This fungus is most often spread by stray cats and pet cats that are allowed outdoors. Learn more about sporotrichosis from cats.
Cause[edit | edit source]
Sporothrix, the fungus that causes sporotrichosis, lives in the environment in soil and on plant matter such as sphagnum moss, rose bushes, hay, or wood. The microscopic fungus can enter the skin through small cuts or scrapes. In rare cases, breathing in the fungus can cause a pulmonary (lung) infection. The type of sporotrichosis found in North America is not contagious and can’t spread from person to person. However, in South America, a type of sporotrichosis caused by Sporothrix brasiliensis spreads through scratches or bites from animals, particularly cats. (This fungal illness is not cat-scratch disease, a bacterial illness spread by cats Рwhich occurs worldwide, wherever cats live.)
Diagnosis & Testing[edit | edit source]
Your healthcare provider will take a small tissue sample (biopsy) of the infected area of the body for laboratory tests. The laboratory will usually perform a fungal culture to find out what is causing the infection. Blood tests can help diagnose severe sporotrichosis, but usually can’t diagnose skin infections.
Treatment[edit | edit source]
Most cases of sporotrichosis only involve the skin or the tissues underneath the skin. These infections are not life-threatening, but must be treated with prescription antifungal medicine for several months. The most common treatment for this type of sporotrichosis is itraconazole, taken by mouth for 3 to 6 months. Supersaturated potassium iodide (SSKI) is another treatment option for skin sporotrichosis. SSKI and azole drugs like itraconazole should not be used if you are pregnant. If you have severe sporotrichosis that affects your lungs, bones, joints, or central nervous system, you’ll probably receive intravenous amphotericin B medicine, which is given through a vein. After the first treatment with amphotericin B, you may receive itraconazole by mouth, for a total of at least 1 year of antifungal treatment. People with sporotrichosis in the lungs may also need surgery to cut away the infected tissue.
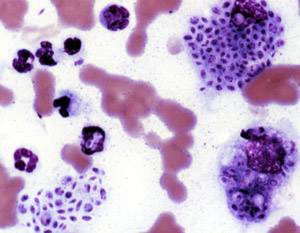
Gallery[edit | edit source]
Sporothrix schenckii PHIL 3943 lores
Buffalo medical journal (1913) (14741044226)
The British journal of dermatology (1888) (14787067013)
- Sporotrichosis by Health in Plain English (with pictures)
- Sporotrichosis by Centers for Disease Control and Prevention (CDC)
- CDC
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD