Dengue fever
(Redirected from Dengue)
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Dengue fever | |
|---|---|
| Synonyms | Breakbone fever, dandy fever |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Fever, headache, muscle pain, joint pain, skin rash |
| Complications | Dengue hemorrhagic fever, dengue shock syndrome |
| Onset | 4–10 days after exposure |
| Duration | 2–7 days |
| Types | N/A |
| Causes | Dengue virus spread by Aedes mosquito |
| Risks | Living or traveling in tropical areas |
| Diagnosis | Blood test |
| Differential diagnosis | N/A |
| Prevention | Mosquito control, vaccine |
| Treatment | Supportive care, intravenous fluids, pain relief |
| Medication | N/A |
| Prognosis | N/A |
| Frequency | 100–400 million cases per year |
| Deaths | 40,000 per year |
Alternate names[edit | edit source]
Dengue hemorrhagic fever; Dengue shock syndrome; Philippine hemorrhagic fever; Thai hemorrhagic fever; Singapore hemorrhagic fever; Hemorrhagic dengue; DF; Dengue virus infection
Definition[edit | edit source]
Dengue fever (DF), caused by dengue virus, is an arboviral disease characterized by an initial non-specific febrile illness that can sometimes progress to more severe forms manifesting capillary leakage and hemorrhage (dengue hemorrhagic fever, or DHF) and shock (dengue shock syndrome, or DSS). File:Symptoms man - dengue.webm
Epidemiology[edit | edit source]
DF is found in the tropics worldwide, especially in Southeast Asia, the Pacific region, and the Americas, with 40% of the global population at risk. An estimated 50 to 100 million cases of DF, 500,000 hospitalizations, and 20,000 deaths occur yearly worldwide.
Cause[edit | edit source]
- Over 25 different viruses cause viral hemorrhagic fever.
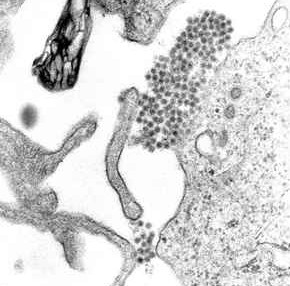
- Dengue virus belongs to the Flaviviridae family, genus Flavivirus. Four distinct serotypes, with significant strain variation, are recognized.
- Dengue is caused by one of any of four related viruses: Dengue virus 1, 2, 3, and 4.  For this reason, a person can be infected with a dengue virus as many as four times in his or her lifetime.
Signs and symptoms[edit | edit source]
- Mild symptoms of dengue can be confused with other illnesses that cause fever, aches and pains, or a rash.
- Graphic of human body showing most common symptom of dengue is fever with any of the following: eye pain, headache, muscle pain, rash, bone pain, nausea/vomiting, joint pain
The most common symptom of dengue is fever with any of the following:
- Nausea, vomiting
- Rash
- Aches and pains (eye pain, typically behind the eyes, muscle, joint, or bone pain)
- Any warning sign
- Symptoms of dengue typically last 2–7 days. Most people will recover after about a week.
Transmission[edit | edit source]
- Dengue viruses are spread to people through the bites of infected Aedes species mosquitoes (Ae. aegypti or Ae. albopictus).
- These mosquitoes typically lay eggs near standing water in containers that hold water, like buckets, bowls, animal dishes, flower pots, and vases.
- These mosquitoes prefer to bite people, and live both indoors and outdoors near people.
- Mosquitoes that spread dengue, chikungunya, and Zika bite during the day and night.
- Mosquitoes become infected when they bite a person infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.
From mother to child
- A pregnant woman already infected with dengue can pass the virus to her fetus during pregnancy or around the time of birth.
- To date, there has been one documented report of dengue spread through breast milk.
- Because of the benefits of breastfeeding, mothers are encouraged to breastfeed even in areas with risk of dengue.
- Dengue in pregnancy
- Rarely, dengue can be spread through blood transfusion, organ transplant, or through a needle stick injury.
Diagnosis[edit | edit source]
Most state health departments and many commercial laboratories perform dengue diagnostic testing. Nucleic acid amplification tests (NAATs)
- For patients with suspected dengue virus disease, NAATs are the preferred method of laboratory diagnosis.
- NAATs should be performed on serum specimens collected 7 days or less after symptom onset.
- Laboratory confirmation can be made from a single acute-phase serum specimen obtained early (≤7 days after fever onset) in the illness by detecting viral genomic sequences with rRT-PCR or dengue nonstructural protein 1 (NS1) antigen by immunoassay.
- Presence of virus by rRT-PCR or NS1 antigen in a single diagnostic specimen is considered laboratory confirmation of dengue in patients with a compatible clinical and travel history.
Serologic tests
- IgM antibody testing can identify additional infections and is an important diagnostic tool. However, interpreting the results is complicated by cross-reactivity with other flaviviruses, like Zika, and determining the specific timing of infection can be difficult.
- Later in the illness (‚â•4 days after fever onset), IgM against dengue virus can be detected with MAC-ELISA. For patients presenting during the first week after fever onset, diagnostic testing should include a test for dengue virus (RT-PCR or NS1) and IgM.
- For patients presenting >1 week after fever onset, IgM detection is most useful, although NS1 has been reported positive up to 12 days after fever onset . In the United States, both MAC-ELISA and RT-PCR are approved as in vitro diagnostic tests.
- IgM in a single serum sample strongly suggests a recent dengue virus infection and should be presumed confirmatory for dengue if the infection occurred in a place where other potentially cross-reactive flaviviruses (such as Zika, West Nile, yellow fever, and Japanese encephalitis viruses) are not a risk.
- PRNTs can resolve false-positive IgM antibody results caused by non-specific reactivity, and, in some cases, can help identify the infecting virus. However, in areas with high prevalence of dengue and Zika virus neutralizing antibodies, PRNT may not confirm a significant proportion of IgM positive results. PRNT testing is available through several state health departments and CDC.
Cross-reactive flaviviruses
- If infection is likely to have occurred in a place where other potentially cross-reactive flaviviruses circulate, both molecular and serologic diagnostic testing for dengue and other flaviviruses should be performed.
- People infected with or vaccinated against other flaviviruses (such as yellow fever or Japanese encephalitis) may produce cross-reactive flavivirus antibodies, yielding false-positive serologic dengue diagnostic test results.
- IgG antibody testing
- IgG detection by ELISA in a single serum sample is not useful for diagnostic testing because it remains detectable for life after a dengue virus infection.
Treatment[edit | edit source]
No treatment: No specific antiviral agents exist for dengue. Supportive care is advised:
- Patients should be advised to stay well hydrated and to avoid aspirin (acetylsalicylic acid), aspirin-containing drugs, and other nonsteroidal anti-inflammatory drugs (such as ibuprofen) because of their anticoagulant properties.
- Fever should be controlled with acetaminophen and tepid sponge baths.
- Febrile patients should avoid mosquito bites to reduce risk of further transmission.
Severe Dengue
- For those who develop severe dengue, close observation and frequent monitoring in an intensive care unit may be required.
- Prophylactic platelet transfusions in dengue patients are not beneficial and may contribute to fluid overload.
- Administration of corticosteroids has no demonstrated benefit and is potentially harmful to patients; corticosteroids should not be used except in the case of autoimmune-related complication (e.g., hemophagocytic lymphohistiocytosis, immune thrombocytopenia purpura).
Prevention[edit | edit source]
Prevent dengue by avoiding mosquito bites.
- All four dengue viruses are spread primarily through the bite of an infected Aedes species (Ae. aegypti and Ae. albopictus) mosquito. These mosquitoes also spread chikungunya and Zika viruses.
- The mosquitoes that spread dengue are found in most tropical and subtropical regions of the world, including many parts of the United States.
- Ae. aegypti and Ae. albopictus bite during the day and night.
- A dengue vaccine is available for use in some parts of the world, including United States territories.
| This article is a medical stub. You can help WikiMD by expanding it! | |
|---|---|
NIH genetic and rare disease info[edit source]
Dengue fever is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Dengue fever
|
Transform your life with W8MD's budget GLP1 injections from $125
W8MD offers a medical weight loss program NYC and a clinic to lose weight in Philadelphia. Our W8MD's physician supervised medical weight loss centers in NYC provides expert medical guidance, and offers telemedicine options for convenience.
Why choose W8MD?
- Comprehensive care with FDA-approved weight loss medications including:
- loss injections in NYC both generic and brand names:
- weight loss medications including Phentermine, Qsymia, Diethylpropion etc.
- Accept most insurances for visits or discounted self pay cost.
- Generic weight loss injections starting from just $125.00 for the starting dose
- In person weight loss NYC and telemedicine medical weight loss options in New York city available
- Budget GLP1 weight loss injections in NYC starting from $125.00 biweekly with insurance!
Book Your Appointment
Start your NYC weight loss journey today at our NYC medical weight loss, and Philadelphia medical weight loss Call (718)946-5500 for NY and 215 676 2334 for PA
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD