Yellow nail syndrome
Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Yellow nail syndrome | |
|---|---|
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Yellow nails, lymphedema, pleural effusion |
| Complications | Respiratory tract infections, bronchiectasis |
| Onset | Usually in adulthood |
| Duration | Chronic |
| Types | N/A |
| Causes | Unknown, possibly genetic |
| Risks | Lymphedema, chronic respiratory conditions |
| Diagnosis | Clinical evaluation, nail biopsy |
| Differential diagnosis | Onychomycosis, psoriasis, chronic bronchitis |
| Prevention | N/A |
| Treatment | Vitamin E, corticosteroids, antibiotics |
| Medication | N/A |
| Prognosis | Variable, often chronic |
| Frequency | Rare |
| Deaths | N/A |
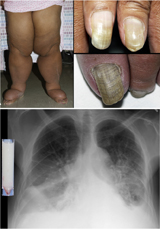
Yellow nail syndrome, also known as "primary lymphedema associated with yellow nails and pleural effusion"
Other Names[edit | edit source]
Lymphedema with yellow nails; YNS
Characteristics[edit | edit source]
Yellow nail syndrome is a very rare disorder characterized by three features:
- yellow nail discoloration,
- respiratory problems, and
- lower limb swelling (lymphedema).
Demographics[edit | edit source]
It usually occurs in people over age 50, but can occur in younger people.
Clinical features[edit | edit source]
In addition to being yellow, nails may lack a cuticle, grow very slowly, and become detached (onycholysis). Respiratory problems may include chronic cough, bronchiectasis, and pleural effusion. Chronic sinusitis may also occur. The cause of yellow nail syndrome remains unknown. It usually occurs on its own, but is sometimes associated with autoimmune disease, lymphatic diseases, or cancers. Some researchers have hypothesized that titanium may play a role in the development of yellow nail syndrome (for example, in dental or joint implants or other environmental exposures). Treatment addresses each symptom present. In some cases, yellow nail syndrome goes away on its own.
Signs and symptoms[edit | edit source]
80%-99% of people have these symptoms
- Bronchiectasis
- Fingernail dysplasia
- Hypoplasia of lymphatic vessels
- Lymphedema
- Toenail dysplasia or Yellow nails
30%-79% of people have these symptoms
- Cough
- Dyspnea
- Pleuritis
- Recurrent respiratory infections
- Rhinitis
- Sinusitis
5%-29% of people have these symptoms
- Biliary tract neoplasm
- Generalised abnormality of skin
- Immunodeficiency
- Neoplasm of the lung
- Nephropathy
- Onycholysis or detachment of nail
- Pulmonary arterial hypertension
- Renal neoplasm
- Sarcoma
Cause[edit | edit source]
- The exact cause of yellow nail syndrome remains unknown. Lymphatic impairment or reduced lymphatic drainage has been proposed, as it may explain lymphedema, pleural effusion, and nail discoloration.
- However, problems with the lymphatic system are not known to cause bronchiectasia and sinusitis.
- Additionally, lymphatic impairment is not easy to confirm.
- While most cases of yellow nail syndrome occur randomly, a few cases have run in families.
- Although this suggests that genetic factors may play a role in some cases, no known genetic factors have been identified.
Rarely, yellow nail syndrome has occurred in people with autoimmune disease, lymphatic diseases, or cancers.
Diagnosis[edit | edit source]
Making a diagnosis for a genetic or rare disease can often be challenging. Medical history, symptoms, physical exam, and laboratory test results are important in order to make a diagnosis.
Testing[edit | edit source]
- Pulmonary function testing can show obstruction of the airways.
- People with pleural effusions may show evidence of restriction in lung volumes due to the fluid.
- Analysis of the fluid in pleural effusions generally shows high levels of protein but low levels of cholesterol and lactate dehydrogenase, but about 30% of effusions are chylous (chylothorax) in that they have the characteristics of lymph.
- A lymphogram may be performed in people with lymphedema.
- This can show both under developed (hypoplastic) lymphatic ducts and dilated ducts.
- Dye may be found in the skin months after the initial test.
- Scintigraphy of lymph flow (lymphoscintigraphy) shows delays in drainage of lymph (sometimes asymmetrically), although this test can also be normal.
Treatment[edit | edit source]
- Yellow nail syndrome management aims to address each of the symptoms.
- Treatment for nail discoloration may include oral vitamin E and/or triazole antifungals.
- Pleural effusion may be treated with surgery.
- Antibiotic prophylaxis may be prescribed for bronchiectasia with chronic mucus production.
- Lymphedema treatment may involve low-stretch bandages and elastic compression garments combined with skin care, exercises and manual lymph drainage as needed.
- In some cases, yellow nail syndrome goes away on its own or when an underlying, associated condition is treated.
Genetics[edit | edit source]
Although it has been described in families, it has been suggested that it might not have a genetic link.
Prognosis[edit | edit source]
People with yellow nail syndrome have been found to have a moderately reduced lifespan compared to people without the condition.
Epidemiology[edit | edit source]
The condition is thought to be rare, with approximately 150 cases described in the medical literature.
Patient Registry[edit | edit source]
- Research is needed to determine the cause of YNS, to identify biomarkers for diagnosis, prognosis and response to therapy, and to find effective treatments.
- Patients, families, and caregivers are encouraged to join the NIH Rare Lung Diseases Consortium Contact Registry.
History[edit | edit source]
The condition was first described in 1964 by London physicians Peter Samman and William White.
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's NYC physician weight loss.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available. Call 718 946 5500.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Contributors: Prab R. Tumpati, MD