Medical cannabis
(Redirected from Canasol)
Medical use of cannabis and its derivatives
| Cannabis |
|---|
|
|


Medical cannabis, also known as medicinal cannabis or medical marijuana (MMJ), refers to the use of the cannabis plant and its cannabinoid compounds for therapeutic or symptomatic treatment. It is prescribed for managing various conditions, though clinical research is still ongoing to assess its safety and efficacy. Due to legal restrictions, research into medical cannabis has historically been limited, resulting in varying levels of regulation and availability across different countries.
Medical Applications[edit | edit source]
Preliminary studies suggest that medical cannabis may help with conditions such as chronic pain, nausea related to chemotherapy, and muscle spasticity in multiple sclerosis. Some research also explores its potential role in neurological disorders, mental health conditions, and pain management.
Chronic Pain[edit | edit source]
Cannabinoids, including tetrahydrocannabinol (THC) and cannabidiol (CBD), interact with the endocannabinoid system, which plays a role in pain modulation. Some studies indicate that medical cannabis may provide relief for neuropathic pain, fibromyalgia, and rheumatic diseases. However, long-term effects and optimal dosages remain uncertain.
Chemotherapy-Induced Nausea and Vomiting[edit | edit source]
Medical cannabis has been used to alleviate chemotherapy-induced nausea and vomiting (CINV). It has been found to be an alternative to traditional antiemetic medications for patients who do not respond well to standard treatments.
Muscle Spasms and Spasticity[edit | edit source]
In multiple sclerosis, cannabis-based treatments have shown promise in reducing spasticity and muscle spasms, leading to improved mobility and quality of life. Some prescription drugs derived from cannabis, such as nabiximols, are approved for this use in specific regions.
Neurological and Psychiatric Conditions[edit | edit source]
Research on cannabis-based therapies for epilepsy, Parkinson’s disease, and Alzheimer’s disease is ongoing. The U.S. Food and Drug Administration (FDA) has approved a CBD-based medication, Epidiolex, for treating Lennox-Gastaut syndrome and Dravet syndrome in children. Studies also explore cannabis' effects on anxiety disorders, depression, and post-traumatic stress disorder.
Adverse Effects[edit | edit source]
The use of medical cannabis can result in both short-term and long-term effects.
Short-Term Effects[edit | edit source]
Common side effects include:
- Dizziness
- Drowsiness
- Increased appetite
- Cognitive impairment
- Hallucinations in high doses
Long-Term Effects[edit | edit source]
Prolonged use may be associated with:
- Memory loss
- Cannabis dependence
- Increased risk of psychosis, particularly in individuals predisposed to schizophrenia
- Cannabinoid hyperemesis syndrome, a condition characterized by recurrent nausea and vomiting
Administration Methods[edit | edit source]
Medical cannabis can be consumed in different forms, each with unique effects on absorption and bioavailability.
- Inhalation – Includes cannabis smoking and vaporization. It provides rapid onset of effects but may have respiratory risks.
- Oral administration – Consists of capsules, tinctures, and cannabis edibles. Effects take longer to manifest but last longer.
- Sublingual administration – Cannabis oils and oromucosal sprays are absorbed through the mucous membranes.
- Topical application – Cannabis-infused topicals, such as creams and transdermal patches, are used for localized relief.
- Suppository administration – Used for patients unable to take cannabis orally.
Legal Status[edit | edit source]
The legality of cannabis for medical use varies across the world. Some countries allow it under strict regulations, while others impose significant restrictions or outright bans.
International Status[edit | edit source]
Countries that have legalized medical cannabis include Canada, Germany, Australia, Israel, and several European Union nations. In Latin America, countries such as Argentina, Chile, and Mexico have established medical cannabis programs.
United States[edit | edit source]
In the United States, medical cannabis is legal in 38 U.S. states and the District of Columbia, but remains a Schedule I controlled substance under federal law. The Rohrabacher–Farr amendment prevents federal intervention in states where medical cannabis is legal.
United Kingdom[edit | edit source]
In the United Kingdom, cannabis-based medicines, including Sativex and Epidiolex, are available by prescription for specific conditions.
Other Countries[edit | edit source]
Some nations, including Japan, Singapore, and the United Arab Emirates, maintain strict bans on medical cannabis. Others permit limited access through special research programs or compassionate use laws.
Pharmacology[edit | edit source]
The cannabis plant contains over 100 different cannabinoids, with THC and CBD being the most studied. These compounds interact with the endocannabinoid system, which influences various physiological functions.
Cannabinoids[edit | edit source]
- Tetrahydrocannabinol (THC) – The primary psychoactive compound, responsible for the "high" effect.
- Cannabidiol (CBD) – Non-psychoactive, with potential anti-inflammatory and neuroprotective properties.
- Cannabigerol (CBG) – A precursor to THC and CBD, being studied for its potential medical applications.
- Cannabinol (CBN) – A byproduct of THC degradation, with mild sedative effects.
Absorption and Metabolism[edit | edit source]
The bioavailability of cannabinoids depends on the route of administration. Inhaled cannabis reaches peak concentrations within minutes, while oral cannabis undergoes extensive first-pass metabolism in the liver, leading to slower but prolonged effects.
History[edit | edit source]
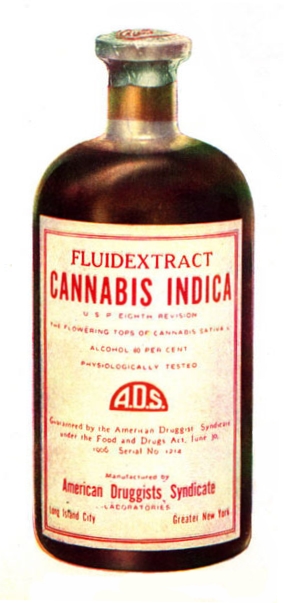
Cannabis has been used medicinally for thousands of years.
Ancient Use[edit | edit source]
- The Ebers Papyrus from Ancient Egypt (circa 1550 BCE) describes cannabis as a treatment for inflammation.
- In China, Shen-Nung documented its therapeutic use around 2700 BCE.
- Greek medicine used cannabis to treat wounds and pain.
Modern History[edit | edit source]
- In the 19th century, cannabis was introduced to Western medicine by William Brooke O'Shaughnessy, an Irish physician.
- The 20th century saw increasing restrictions, culminating in the Marihuana Tax Act of 1937 in the United States.
- The 1970 Controlled Substances Act classified cannabis as a Schedule I drug, restricting research.
- In 1996, California became the first U.S. state to legalize medical cannabis with Proposition 215.
- Canada became the first country to legalize medical cannabis nationwide in 2001.
Society and Culture[edit | edit source]
Public attitudes toward medical cannabis have shifted significantly in recent years, with growing support for its therapeutic applications. Various medical organizations, including the American Nurses Association and the American Academy of Family Physicians, support rescheduling cannabis to allow further research.
Future Research[edit | edit source]
Despite growing acceptance, medical cannabis research faces challenges due to legal barriers and variability in cannabis-based treatments. Ongoing studies aim to clarify its role in managing pain, neurological disorders, and mental health conditions.
| Cannabis | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
*
|
Search WikiMD
Ad.Tired of being Overweight? Try W8MD's physician weight loss program.
Semaglutide (Ozempic / Wegovy and Tirzepatide (Mounjaro / Zepbound) available.
Advertise on WikiMD
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
- Pages with script errors
- Use American English from March 2025
- Articles with invalid date parameter in template
- All Wikipedia articles written in American English
- Medicinal use of cannabis
- Antiemetics
- Antioxidants
- Biologically based therapies
- Herbalism
- Medical ethics
- Medicinal plants
- Pharmaceuticals policy
- Pharmacognosy
Contributors: Prab R. Tumpati, MD